RECIL 2017:淋巴瘤试验中疗效评估新标准
2018-07-10 MedSci MedSci原创
美国纪念斯隆凯特琳癌症中心Anas Younes等近期代表国际工作组报告了一个代号为RECIL 2017的新标准,用以评估淋巴瘤临床试验中的疗效,旨在解决常用实体瘤疗效评价标准(RECIST)中的部分问题。(Ann Oncol. 2017年4月3日在线版)目前,标准的淋巴瘤疗效评价准则为“Lugano标准”,其基础是18F FDG-PET扫描结果或CT扫描上的肿瘤二维测量结果。而RECIST标准则
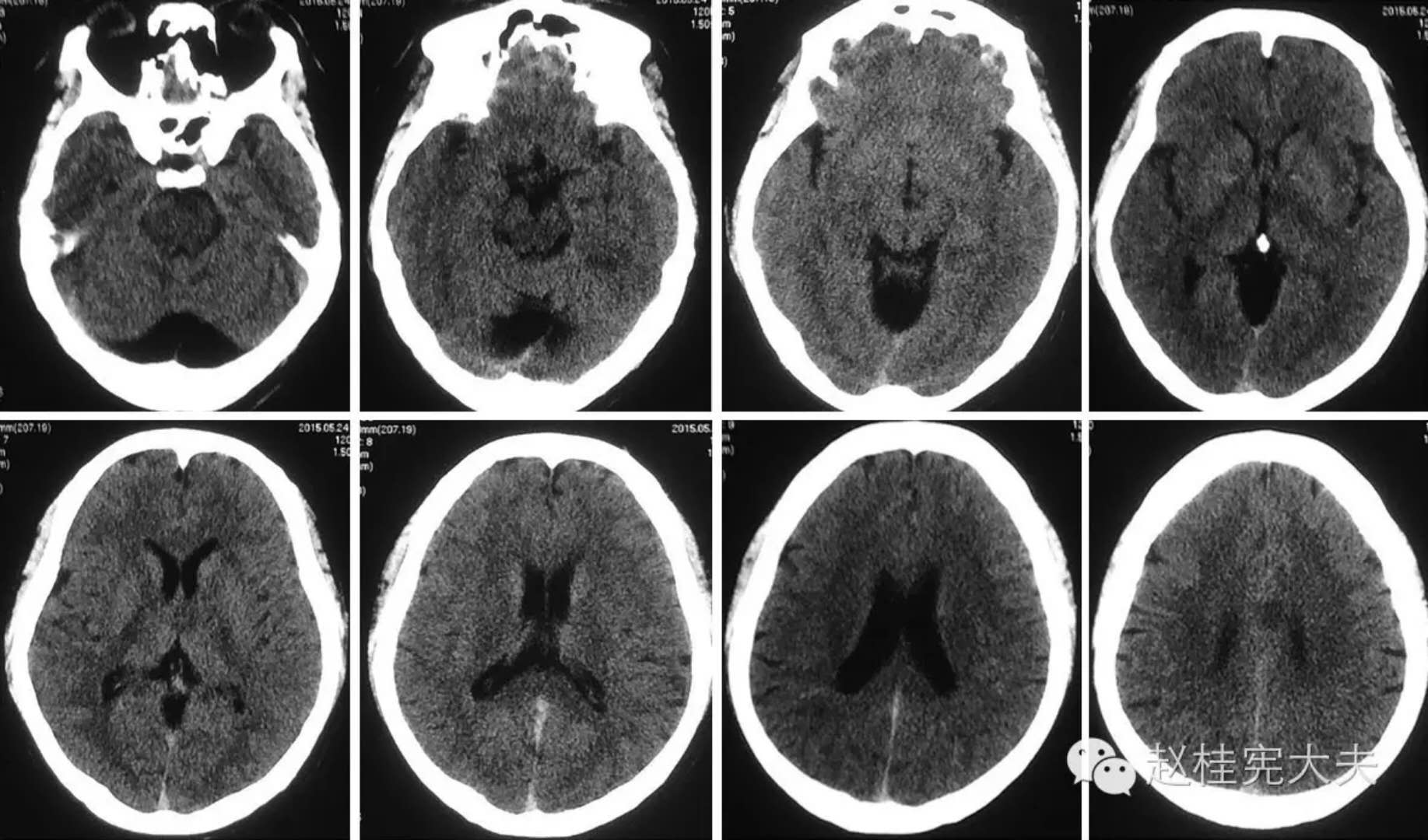
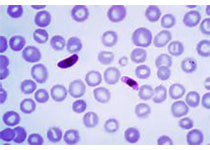
美国纪念斯隆凯特琳癌症中心Anas Younes等近期代表国际工作组报告了一个代号为RECIL 2017的新标准,用以评估淋巴瘤临床试验中的疗效,旨在解决常用实体瘤疗效评价标准(RECIST)中的部分问题。(Ann Oncol. 2017年4月3日在线版)目前,标准的淋巴瘤疗效评价准则为“Lugano标准”,其基础是18F FDG-PET扫描结果或CT扫描上的肿瘤二维测量结果。而RECIST标准则是基于一维的肿瘤测量结果。一些来自学术中心、制药企业、放射科的专家和统计学家共同组成了一个国际淋巴瘤专家组,旨在协调使用RECIST标准评价淋巴瘤疗效时存在的问题。他们首先假设,一维测量在评估疗效时与Lugano标准获得相似的结果。然后,研究者们自10个多中心临床试验中入组2983例成人和儿童淋巴瘤患者,获取了47 828幅影像检测结果,用以分析验证假设的正确性。结果发现,在淋巴瘤临床试验中评估肿瘤负荷可使用三个靶病灶最长直径之和来衡量,同时还需包含一个轻微缓解的分类。RECIL 2017疗效评价标准的要点如下。评估肿瘤负荷在淋巴瘤临床试验中,肿瘤负荷的评估可使用最长直径的总和来进行。针对弥漫
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









谢谢分享
126
#新标准#
137
#疗效评估#
129
谢谢梅斯提供这么好的信息,学到很多
109
学习一下谢谢.谢谢分享
135