NEJM:Jakavi(ruxolitinib)治疗急性移植物抗宿主病,优于现有更佳疗法
2020-04-23 Allan MedSci原创
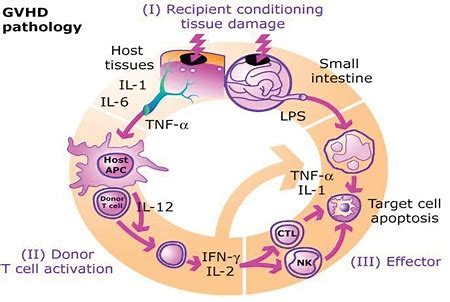
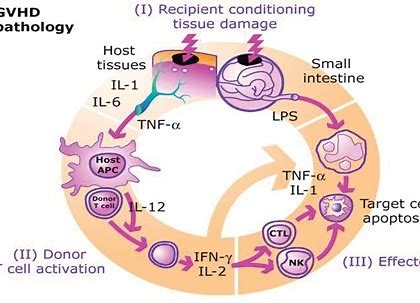
今天发表于《新英格兰医学杂志》的III期REACH2研究表明,与现有最佳药物相比,Jakavi(ruxolitinib)改善了激素抵抗性急性移植物抗宿主病(GvHD)患者的一系列疗效指标。
今天发表于《新英格兰医学杂志》的III期REACH2研究表明,与现有最佳药物相比,Jakavi(ruxolitinib)改善了激素抵抗性急性移植物抗宿主病(GvHD)患者的一系列疗效指标。REACH2是第一个达到主要终点的急性GvHD的III期研究。REACH2试验的详细数据将在8月30日至9月2日在西班牙马德里举行的欧洲血液和骨髓移植学会(EBMT)年度会议上介绍。
相比于现有最佳药物,接受Jakavi治疗的患者在第28天具有更高的总缓解率(ORR)(62%比39%,p<0.001);接受Jakavi治疗的患者在8周时的ORR显著更高(40%比22%,p<0.001)。此外,Jakavi的FFS比现有最佳药物更长(5.0个月比1.0个月)。
该研究的主要领导者说:“急性移植物抗宿主病患者面临着生命威胁和有限的治疗选择,特别是对于激素抵抗性患者。来自REACH2的数据表明,Jakavi优于当前最佳药物。这些证据表明,在这种难以治疗的情况下,靶向JAK途径可以成为一种有效的策略”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#植物#
53
#JAK#
35
#宿主#
42
#移植物抗宿主病#
52
#ruxolitinib#
43
#移植物#
39
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
49