Med: 震惊!哈佛大学超7万样本研究:麻腮风和百白破疫苗竟能对重症新冠患者提供保护!
2021-09-03 生物探索 生物探索
哈佛大学的一项最新研究发现,麻腮风和百白破疫苗能引发人体产生交叉反应性记忆T细胞,识别新冠病毒中的抗原,加强对COVID-19 的保护作用。
半个世纪以来,儿童早期接种的麻疹-腮腺炎-风疹疫苗(MMR)和每10年接种一次的伤风-白喉-百日咳 (Tdap)疫苗已安全地提供给全球数亿人,并成功降低了全世界相关疾病的发病率。近日,哈佛大学的一项最新研究发现,这些疫苗还有一个意想不到的功能,它们竟然能引发人体产生交叉反应性记忆T细胞,识别新冠病毒中的抗原,加强对COVID-19 的保护作用。相关研究以“Protective Heterologous T Cell Immunity in COVID-19 Induced by MMR and Tdap Vaccine Antigens”为题发表于《Med》杂志。
IFN-γ作为免疫活性细胞分泌的细胞因子在诱导抗病毒免疫中起着重要的免疫调理作用,包括激活细胞毒性T淋巴细胞(CTL)、自然杀伤细胞(NK)和吞噬细胞等,而在疫苗免疫后机体产生IFN-γ的水平实际上反映辅助性T细胞的活动。因此,检测IFN-γ的水平就是间接地检测辅助性T细胞活性。
目前,检测IFN-γ的水平已经逐渐代替各种传统的细胞免疫检测手段,成为检测细胞免疫效果的一种重要方法。特别是IFN-γ ELISpot检测法,它可以有效检测和评价疫苗细胞免疫,逐渐成为疫苗引起的细胞免疫效应评估的“金标准”。因此,为了验证MMR和Tdap疫苗对新冠病毒的额外保护作用,研究团队将载有SARS-CoV-2、MMR 或 Tdap 抗原的抗原呈递细胞(APC)与自体T细胞的共培养,同时使用IFN-γ ELISpot检测法和流式细胞术来检测T细胞活性。
研究发现,在新冠病毒感染个体中,T细胞对SARS-CoV-2、MMR和Tdap疫苗蛋白的应答高度相关。这说明存在对SARS-CoV-2抗原,以及MMR和Tdap疫苗抗原产生相同反应的特异性免疫。
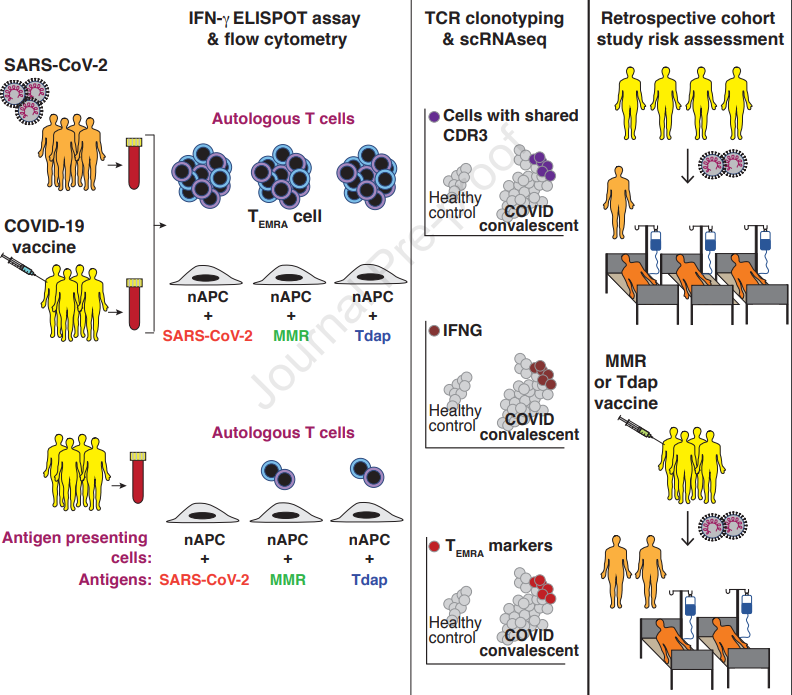
(图注:试验流程图)
在体外试验取得良好结果的基础上,研究人员与世界最著名医疗机构“克利夫兰医学中心”合作,使用重叠倾向评分加权统计方法,对来自俄亥俄州和克利夫兰医学中心的 75000 多名在2020年3月8日至2021年3 月31日期间检测出COVID-19阳性患者的临床数据进行回顾性队列分析。流行病学的一系列证据表明,接种过MMR疫苗的患者住院率降低了38%,ICU入住率及死亡率降低了32%。受新冠肺炎的影响,人们的常规疫苗接种量显着减少,该研究结果强调了对儿童和成人进行常规疫苗接种的重要性。
然而,尽管MMR和Tdap疫苗不能取代传统的新冠疫苗,但与单独使用新冠疫苗相比,MMR和Tdap疫苗或能针对尖峰变异体,为人体提供更强、更持久的保护。
原始出处:
Vijayashree Mysore, Xavier Cullere. Protective Heterologous T Cell Immunity in COVID-19 Induced by MMR and Tdap Vaccine Antigens. Med, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新冠患者#
77
#百白破#
81
#样本#
70
#哈佛#
75
#Med#
70
学习。
80
新冠肺炎,疫情何时才能消失
90