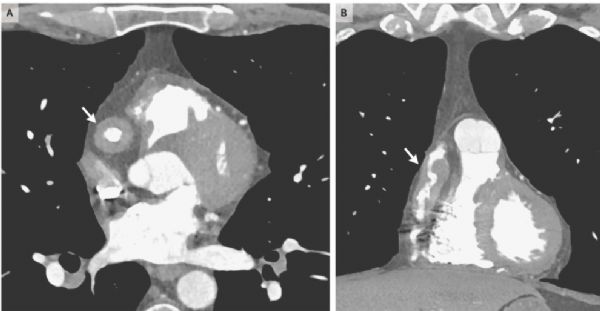
NEJM:IgG4相关疾病中的冠状动脉炎-病例报道
2019-05-30 xing.T 网络
推测这些异常发生在活动性疾病的早期阶段并代表损伤,而不是活跃的IgG4相关疾病。该患者开始接受低剂量阿司匹林治疗。在4个月后的随访检查中,患者仍无症状。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉炎#
0
学习了,谢谢分享
115
#IgG4#
86
#IgG4相关疾病#
78
#IgG#
69
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
71