Hypertension:子宫内膜异位症与高胆固醇血症或高血压之间有何关系?
2017-05-31 xing.T MedSci原创
在这项大型队列研究中,经腹腔镜确诊的子宫内膜异位症与高胆固醇血症和高血压风险增加之间存在前瞻性的相关性。相反,高胆固醇血症和高血压也与较高的经腹腔镜确诊的子宫内膜异位症的发生风险之间存在前瞻性的相关性。
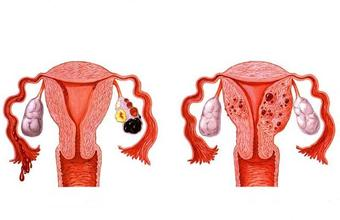
以激素或慢性全身炎症环境改变为特征的子宫内膜异位症可能导致高胆固醇血症和高血压的发生风险增高。相反,由高血压引起的高胆固醇血症中低密度脂蛋白升高和慢性全身性炎症升高可能增加子宫内膜异位症的发生风险。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员在一项大型前瞻性队列研究中评估了腹腔镜确诊的子宫内膜异位症与高胆固醇血症和高血压之间的关系。
在1989年,研究人员对116430名年龄在25至42岁的女护士进行了基础问卷调查,并被随访了20年。采用多变量Cox比例风险模型进行分析。在1989年,有4244名参与者经腹腔镜确诊为子宫内膜异位症患者,91554名女性无子宫内膜异位症。
在调整人口统计学指标、体格发育指标、家组史、生殖情况、饮食习惯和生活方式的危险因素后,研究人员比较了经腹腔镜确诊的子宫内膜异位症妇女与无子宫内膜异位症的妇女,发现其高胆固醇血症发生的相对危险度为1.25(95%可信区间为1.21-1.30),发生高血压的相对危险度为1.14(95%可信区间为1.09-1.18)。
相反,高胆固醇血症女性与无高胆固醇血症的妇女相比,发生经腹腔镜确诊的子宫内膜异位症相对风险为1.22(95%可信区间为1.15-1.31),高血压女性与无高血压的妇女相比,其相对风险为1.29(95%可信区间为1.18-1.41)。经腹腔镜确诊的子宫内膜异位症与高胆固醇血症或高血压之间的相关性强弱程度在≤40岁的女性中最强,随年龄增长其相关性有所减弱(P<0.001)。研究人员发现约45%的子宫内膜异位症与高胆固醇血症和高血压之间的相关性可以通过子宫内膜异位症诊断后的治疗因素来解释,包括较高的子宫/卵巢切除频率以及手术年龄较早。
在这项大型队列研究中,经腹腔镜确诊的子宫内膜异位症与高胆固醇血症和高血压风险增加之间存在前瞻性的相关性。相反,高胆固醇血症和高血压也与较高的经腹腔镜确诊的子宫内膜异位症的发生风险之间存在前瞻性的相关性。
原始出处:
Fan Mu, et al. Association Between Endometriosis and Hypercholesterolemia or Hypertension.Thrombosis and Haemostasis.2017. https://doi.org/10.1161/HYPERTENSIONAHA.117.09056
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TENS#
39
#内膜#
38
#子宫内膜异位#
0
学习了谢谢分享
70
#PE#
47
#高胆固醇血症#
41
#Hypertension#
26
会关注这类病人,学习了,谢谢!
65
谢谢分享,学习了
73
学习
64