干货!系统性红斑狼疮3大分类标准怎么选,这篇文章说清楚了
2021-11-15 Shielry MedSci原创
三大系统性红斑狼疮标准怎么选?新的标准一定更好吗?
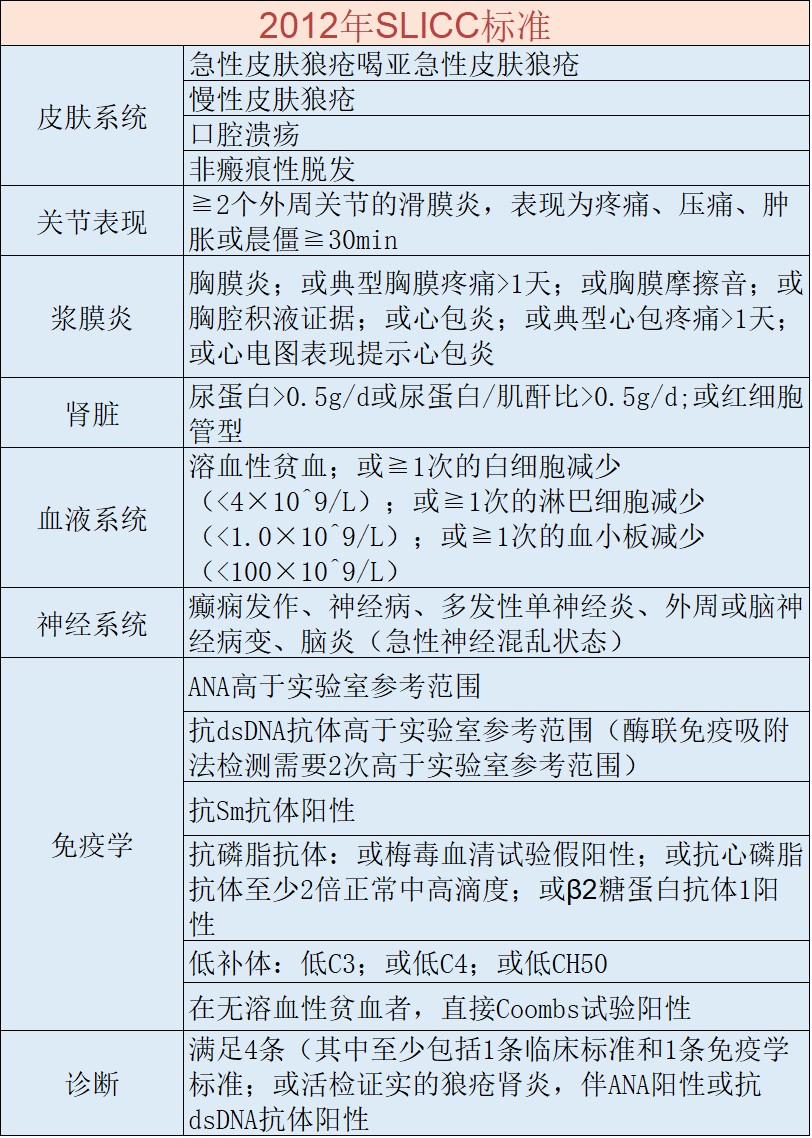
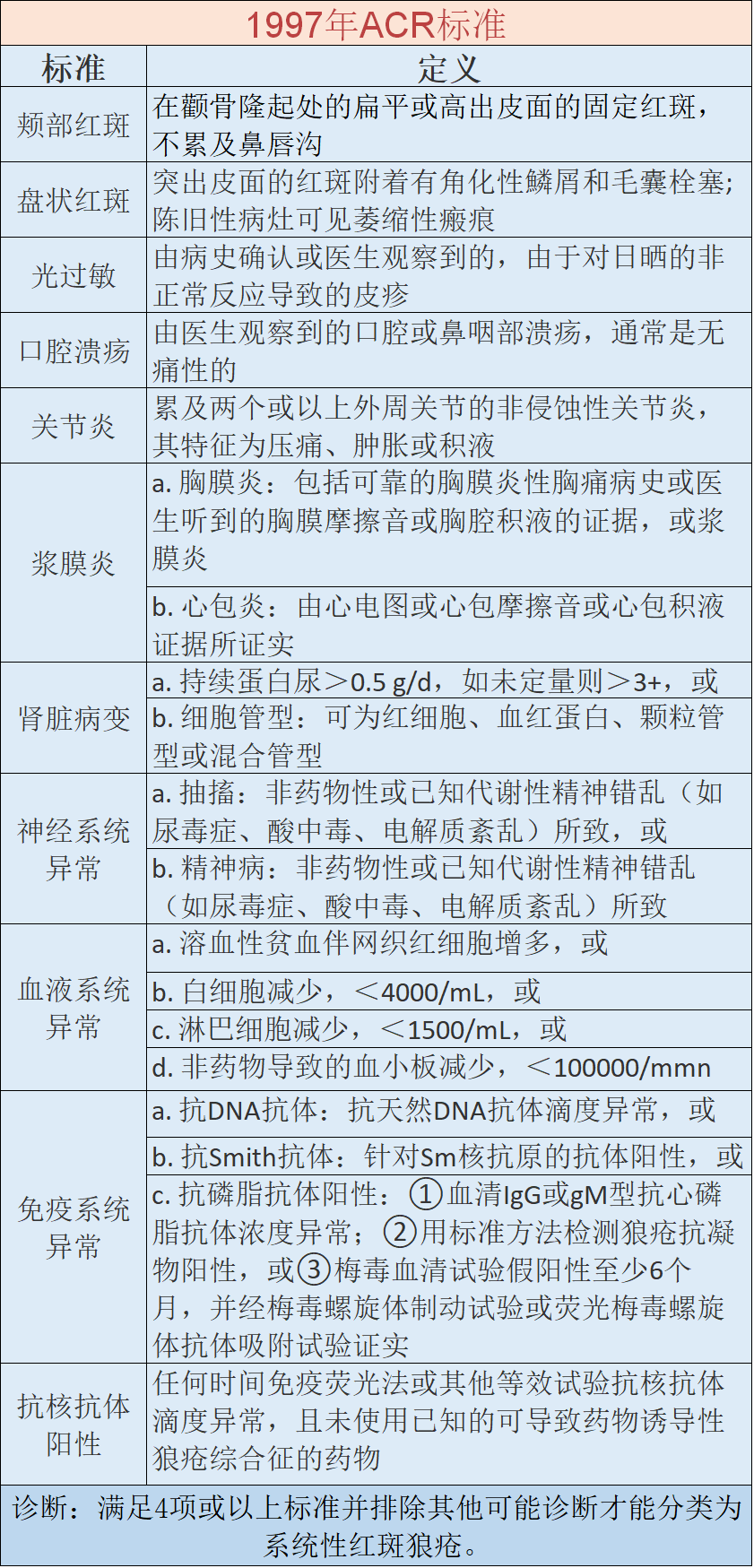
从1997年ACR标准的提出到2012年的SLICC诊断标准以及最新的19年EULAR/ACR标准,他们的具体内容和特异性以及敏感性如何呢? 2019年EULAR/ACR 2020年《2020中国系统性红斑狼疮诊疗指南》中推荐用2012年国际狼疮研究临床协作组(SLICC)或2019年EULAR/ACR 制定的SLE分类标准对疑似SLE者进行诊断。 2019年EULAR/ACR指南采用入围与分类双重标准。将ANA阳性作为SLE分类诊断的“入围”标准,ANA阴性则不考虑诊断SLE。因为但在特定条件下,ANA阴性的SLE几乎不存在。 最新的验证队列研究显示,此分类的敏感性为96%,特异性为93%,均为最优。 2012年SLICC标准 2012年的SLICC分类标准其更加强调临床表现和免疫学指标相结合,取消了部分特异性和敏感性不高的临床表现,且更重视系统受累,提高了肾活检在诊断中的重要性。 针对新标准的诊断准确性研究显示,此SLE分类标准的敏感性为100%,特异性分别为 75%。显示成人 SLE 中2012 年 SLICC 分类标准相对最优。 1997年EULAR/ACR 1997年美国风湿病学会(ACR)分类标准是世界范围内最广泛应用于分类诊断SLE的标准。 其校正之后的特异性和敏感性分别为0.93和0.83,由于敏感性相对较低,容易漏诊,不利于早期诊断。 怎样选择? 目前仅有1997年ACR的SLE分类标准曾在我国SLE人群中进行过验证,结果显示该标准对我国SLE患者具有良好的适用性。新的标准(2012年SLICC、2019年EULAR/ACR)在我国仍然需要更多的数据来验证新SLE标准的适用性。 最新的中国指南也推荐采用新的标准(2012年SLICC/2019 年EULAR/ACR)来进行SLE的诊断。 2012的SLICC标准有虽然有着较高的敏感度,但是特异性较低。 2019年的诊断标准不能诊断 ANA 持续阴性的 SLE,虽然这部分患者并不多见,但也需要探讨其他分类标准的可能性。 2019年的标准对于儿童特异性较低,有研究证实需要将19年的标准≥10分提高到≥13分,则可将其特异度提高到与ACR 1997和SLICC 2012标准相同的水平。 临床医生在选择诊断标准的时候还需要综合考虑,不能只选用最新的标准。必要的时候可以全都要。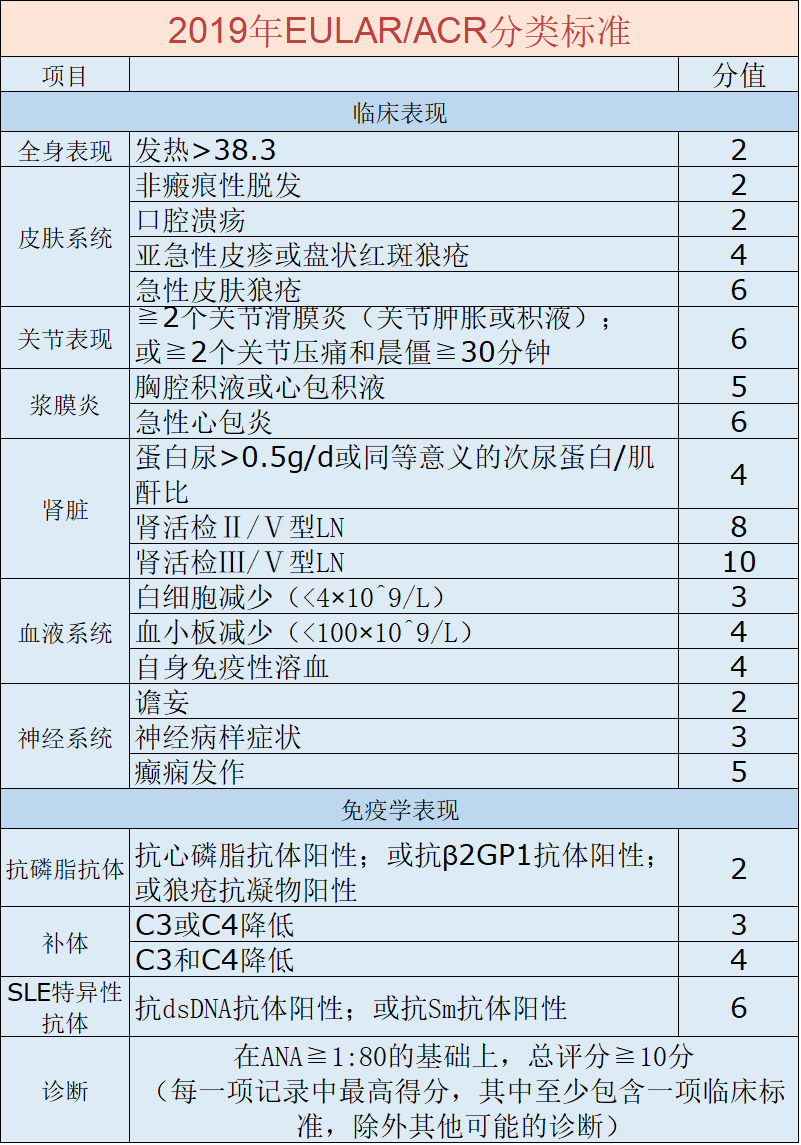
参考文献
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
50
#系统性#
70
#狼疮#
81
#分类标准#
63
#红斑#
62
学习了
77