Front Oncol:PD-1抑制剂nivolumab(纳武利尤单抗)治疗NSCLC患者的长期生存疗效和血液学标志物的探索
2021-12-14 yd2015 MedSci原创
研究表明,真实世界中nivolumab治疗晚期NSCLC的疗效与临床研究一致。6个月时获得应答或稳定患者的生存延长。同时也鉴别出一个预后指标CLAS。
肺癌是全球癌症相关死亡的主要原因。非小细胞肺癌(NSCLC)是其中的重要类型。免疫检查点抑制剂(ICI)治疗晚期NSCLC研究表示,在一线铂类化疗失败后,PD-1抑制剂nivolumab(纳武利尤单抗)治疗NSCLC患者的生存率优于多西他赛。但是,并不是所有患者都可以从nivolumab治疗中获益。因此,鉴别出有效的分子标志物来识别获益人群就尤其重要。来自以色列的学者开展了真实世界研究,评估nivolumab在NSCLC患者的长期生存疗效以及血液学标志物的探索。相关结果发表在Frontiers in Oncology杂志上。
我们对2015-2016年间在以色列三家癌症中心开始使用nivolumab治疗的108例晚期NSCLC患者进行了回顾分析,并对这些患者进行了实验室检测。收集的数据包括性别、年龄、ECOG-PS、组织学和既往治疗线数。采集基线血液检测结果:绝对淋巴细胞和中性粒细胞计数(ANC)、白细胞(WBC)、血红蛋白、血小板、白蛋白和乳酸脱氢酶(LDH)。计算中性粒细胞/淋巴细胞比值及衍生NLR (dNLR = (ANC/[WBC-ANC]))。6个月时的疾病控制(DC6)定义为在nivolumab治疗的6个月时肿瘤缩小或疾病稳定。使用Cox比例风险模型检测临床/实验室变量与生存之间的关联。
本研究共纳入108例接受nivolumab治疗的患者,其中大部分为男性(65%)。在研究队列中,35例(32.4%)患者实现了DC6。非DC6组的ECOG-PS高于DC组(p=0.030)。中位随访时间为48.7个月(IQR 47.4-53.0)。
整个研究人群的中位OS为5.4个月(95% CI 3.9-7.4)。1年、2年、3年和4年的OS率分别为34%、27%、19%和16%。
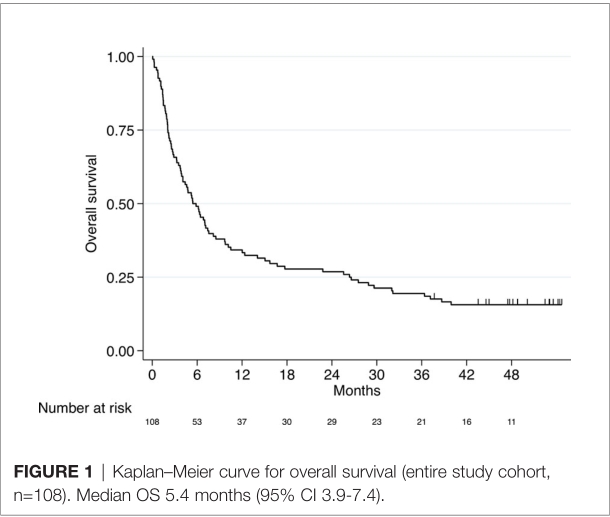
总体人群的OS
在实现DC6的患者中,46%的患者在数据截止时存活,而未实现DC6的患者只有1%存活。此外,与无DC6的患者相比,DC6患者的OS更长(HR 0.12, 95%CI 0.07-0.21, p<0.001)。
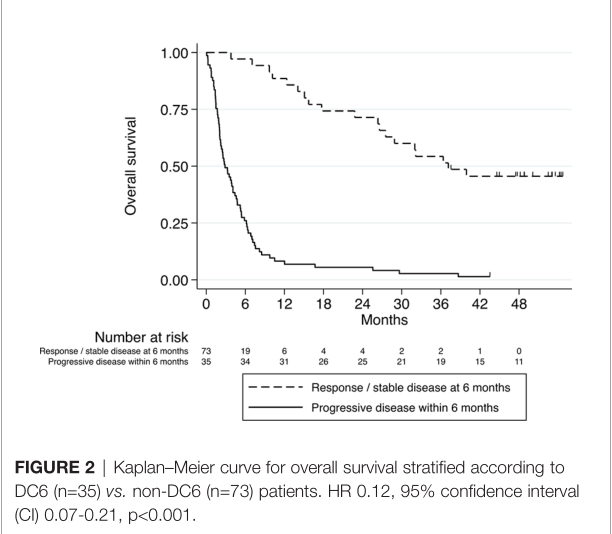
DC6和非DC6患者的OS
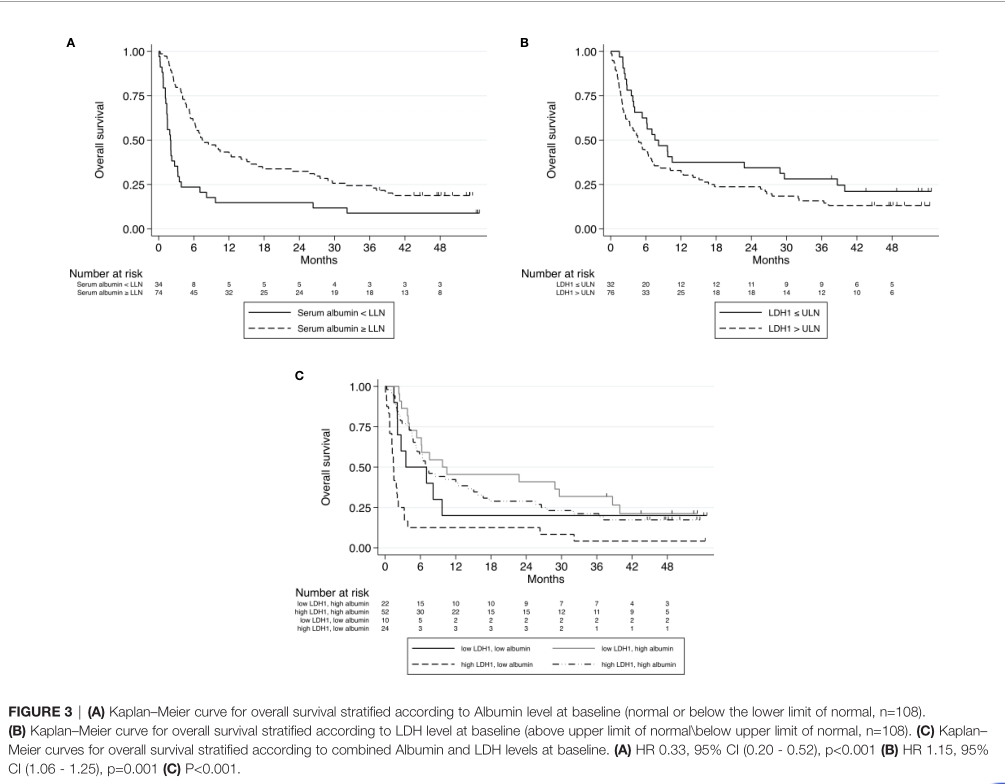
单因素分析,ECOG-PS及基线WBC、ANC、NLR、dNLR、LDH、白蛋白值与OS显著相关。多因素分析,dNLR、白蛋白和LDH与OS显著相关。高dNLR、低白蛋白和高LDH是较差的生存相关。
研究发现基线LDH和白蛋白水平与生存最显著相关。我们试图通过结合这两个变量产生一个预测评分,将其命名为CLAS。CLAS包括四组预后患者:高LDH +低白蛋白(CLA 0),低LDH +低白蛋白(CLA 1),高LDH +高白蛋白(CLA 2),低LDH +高白蛋白(CLA 3)。实际上,CLA 0患者的预后最差,CLA 2患者的预后好于CLA 1患者。
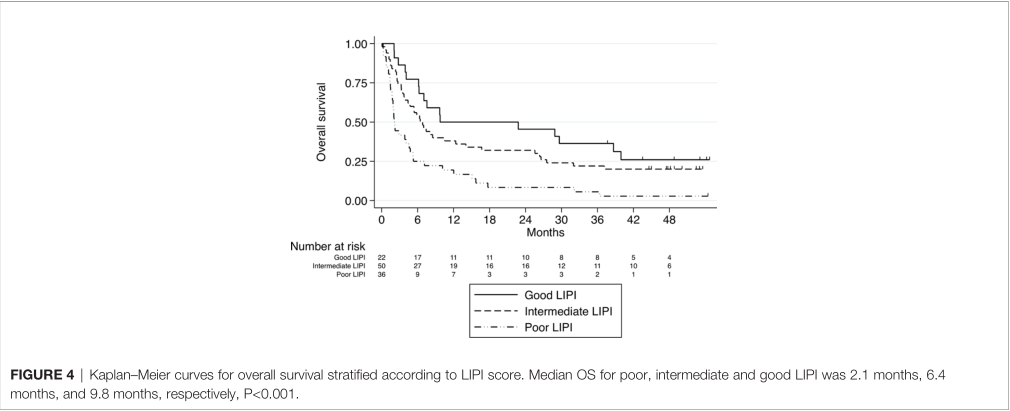
肺免疫预后指数(LIPI)是OS独立预后因素。较差、中等和良好LIPI患者的中位OS分别为2.1个月,6.4个月和9.8个月。
综上,研究表明,真实世界中nivolumab治疗晚期NSCLC的疗效与临床研究一致。6个月时获得应答或稳定患者的生存延长。同时也鉴别出一个预后指标CLAS。
原始出处:
Daher S, Lawrence YR, Dudnik E, Hanovich E, Urban D, Peled N, Navon R, Leibowitz R, Hammerman A, Battat E, Gottfried T, Onn A and Bar J (2021) Nivolumab in Non-Small Cell Lung Cancer: Real World Long-Term Survival Results and Blood-Based Efficacy Biomarkers. Front. Oncol. 11:625668. doi: 10.3389/fonc.2021.625668
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
64
#SCLC患者#
80
#mAb#
89
#抑制剂#
65
#标志物#
63
#NIV#
55
#PD-1抑制剂#
57
#NSCLC患者#
65
#血液学#
82
#长期生存#
69