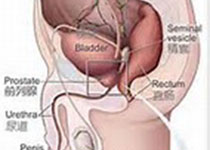
Prostate Cancer P D:患者为中心的前列腺活检报告的发展和比较效果研究
2019-09-13 AlexYang MedSci原创
前列腺活检病理报告是一种用于诊断为前列腺癌患者进行决策的重要文件,然而,报告的内容超出了大多数患者的健康认知情况。最近,有研究人员探索了创建和比较患者为中心的前列腺活检报告与标准报告之间的效果情况。研究人员选择了一级和二级格林森评分以及阳性病灶数目作为报告的最重要内容。患者在风险分类中更倾向于叙述设计、非威胁性语言和信息。在标准报告组中,87%(40/46)的患者完成了起始评估;患者为中心的小组中
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Prostate Ca#
60
#前列腺活检#
71
#活检#
52
#ROS#
62
#PRO#
59
学习了,谢谢分享
130
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
110