Cell Death Dis:鼠尾草酚可抑制炎性小体活化,或可用于治疗相关疾病
2020-04-25 QQY MedSci原创
鼠尾草酚可抑制炎性小体的活化,或可作为治疗炎性小体介导的炎症相关疾病的安全有效的候选药物。
既往研究发现,炎症小体能够参与各种代谢类疾病及炎症相关疾病。在模拟各种人类疾病的动物模型中,炎症小体的药理抑制剂均产生显著的治疗效果。因此,炎症小体被广泛认为是治疗多种疾病的新靶标。
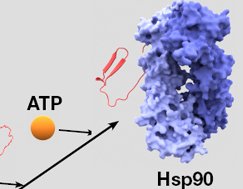
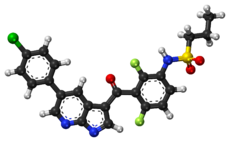
在该研究中,研究人员发现鼠尾草酚(carnosol)可以通过直接靶向HSP90(热休克蛋白90)来抑制NLRP3炎性小体的活化,进而对炎性小体介导的相关疾病起到治疗作用。
研究数据表明,鼠尾草酚能够抑制原代小鼠BMDM细胞(骨髓源性巨噬细胞)、THP-1细胞及hPBMC(人外周血单核细胞)中的NLRP3炎性小体的活化。
机制研究发现,鼠尾草酚通过与HSP90结合抑制其ATPase酶活性并抑制炎性小体的活化过程。体内实验结果表明,在NLRP3炎性小体介导的疾病(包括内毒素血症及非酒精性脂肪性肝炎[NASH])小鼠模型中鼠尾草酚具有显著的治疗作用。
此外,研究人员还发现对小鼠进行持续两周的鼠尾草酚(120 mg/kg,1/日,腹腔注射)治疗,给药小鼠表现出良好的耐受性。
综上,研究结果揭示了鼠尾草酚可抑制炎性小体的活化,或可作为治疗炎性小体介导的炎症相关疾病的安全有效的候选药物。
原始出处:
Shi et al. Carnosol inhibits inflammasome activation by directly targeting HSP90 to treat inflammasome-mediated diseases. Cell Death and Disease (2020) 11:252
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
52
#鼠尾草酚#
57
#CEL#
56
#炎性小体#
104
#Dis#
44
#Death#
45