Nature Communications:监测肿瘤状态的特殊基因
2015-02-05 佚名 生物谷
近日,刊登在国际杂志Nature Communications上的一篇研究论文中,来自西奈山医疗中心(Mount Sinai Medical Center)的研究人员通过研究发现两种癌症药物可以开启特殊基因的表达,而这种特殊基因则可以告知肿瘤细胞使其处于休眠状态。 文章中研究者表示,当名为NR2F1的基因开启后其就会重编程肿瘤细胞使其处于休眠状态;而当该基因的表达关闭后肿瘤细胞就会开始分裂并且发
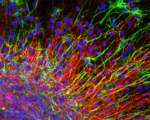
近日,刊登在国际杂志Nature Communications上的一篇研究论文中,来自西奈山医疗中心(Mount Sinai Medical Center)的研究人员通过研究发现两种癌症药物可以开启特殊基因的表达,而这种特殊基因则可以告知肿瘤细胞使其处于休眠状态。
文章中研究者表示,当名为NR2F1的基因开启后其就会重编程肿瘤细胞使其处于休眠状态;而当该基因的表达关闭后肿瘤细胞就会开始分裂并且发生异常生长,从而潜在地使休眠中的细胞迅速生长成为肿瘤,并且发生全身性的转移。研究者表示,将抗癌药物氮杂胞苷和类维生素A进行结合就可以明显增加肿瘤细胞中活性NR2F1的水平。
NR2F1作为肿瘤细胞生长的主要调节基因,其影响着决定细胞是否处于休眠的许多基因的表达;本文研究显示,基因NR2F1在人类胚胎干细胞中发挥着长期的控制作用,在干细胞中其可以指挥细胞停止生长并且变成对生命活动重要的细胞,而NR2F1的这种功能也使其对肿瘤细胞可以施加较长的控制效应,当癌细胞从原发性位点增殖扩散后NR2F1就会促进癌细胞保持休眠状态。
Aguirre-Ghiso教授说道,我们的研究揭示了为何有些肿瘤细胞在扩散到全身后依然会数年保持休眠状态,而为何有些肿瘤细胞却会引发严重的疾病。药物氮杂胞苷和类维生素A可以抑制肿瘤细胞发生快速增殖,从而恢复正常细胞的功能,而一些活性的肿瘤则会抑制关闭肿瘤生长的基因的表达;如今研究人员已经拥有大量的证据可以证明已知抗癌药物的结合具有明显潜在的抗癌效应。
原始出处
Sosa MS1, Parikh F2, Maia AG3, Estrada Y1, Bosch A1, Bragado P1, Ekpin E1, George A1, Zheng Y4, Lam HM5, Morrissey C5, Chung CY3, Farias EF6, Bernstein E7, Aguirre-Ghiso JA8.NR2F1 controls tumour cell dormancy via SOX9- and RARβ-driven quiescence programmes.Nat Commun. 2015 Jan 30

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#COMMUN#
50
#Nat#
54
已阅
193
#Nature Communications#
63