AAOS指南(2022)|关于桡骨远端骨折的7条临床操作建议
2022-04-17 网络 网络
桡骨远端骨折(distal radius fracture, DRF)是临床最常见的骨折之一,发病率呈双峰分布,占青少年骨折的25%及老龄患者骨折的18%。
查看指南原文:2020 AAOS/ASSH临床实践指南:桡骨远端骨折的管理(概要)
桡骨远端骨折(distal radius fracture, DRF)是临床最常见的骨折之一,发病率呈双峰分布,占青少年骨折的25%及老龄患者骨折的18%。
2022年,美国骨科医师协会(The American Academy of Orthopaedic Surgeons,AAOS)与手外科医师协会(The American Society for Surgery of the Hand,ASSH)联合推出了桡骨远端骨折的临床操作指南,包含7条建议,供临床参考。
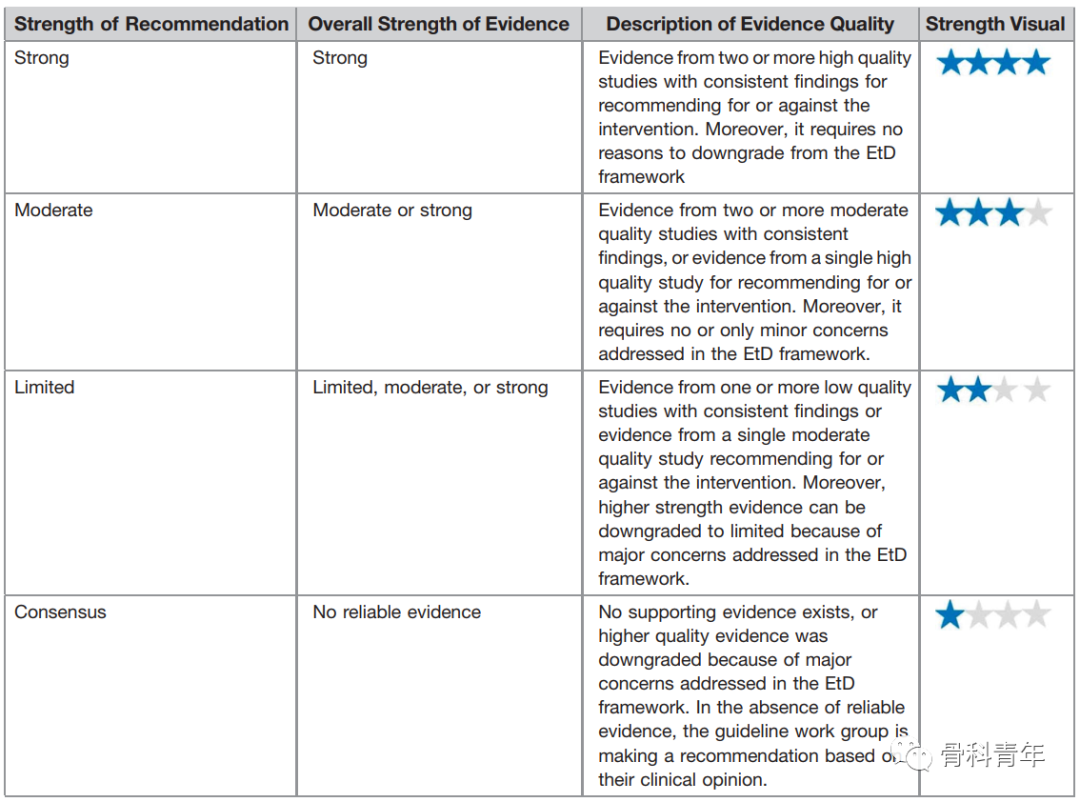
所有的推荐根据证据等级划分:
七条具体建议
一. 关节镜辅助(arthoscopic assistance)
在治疗桡骨远端骨折时,关节镜辅助与非关节镜辅助在治疗结果上无明显差异。(证据指数:中等)

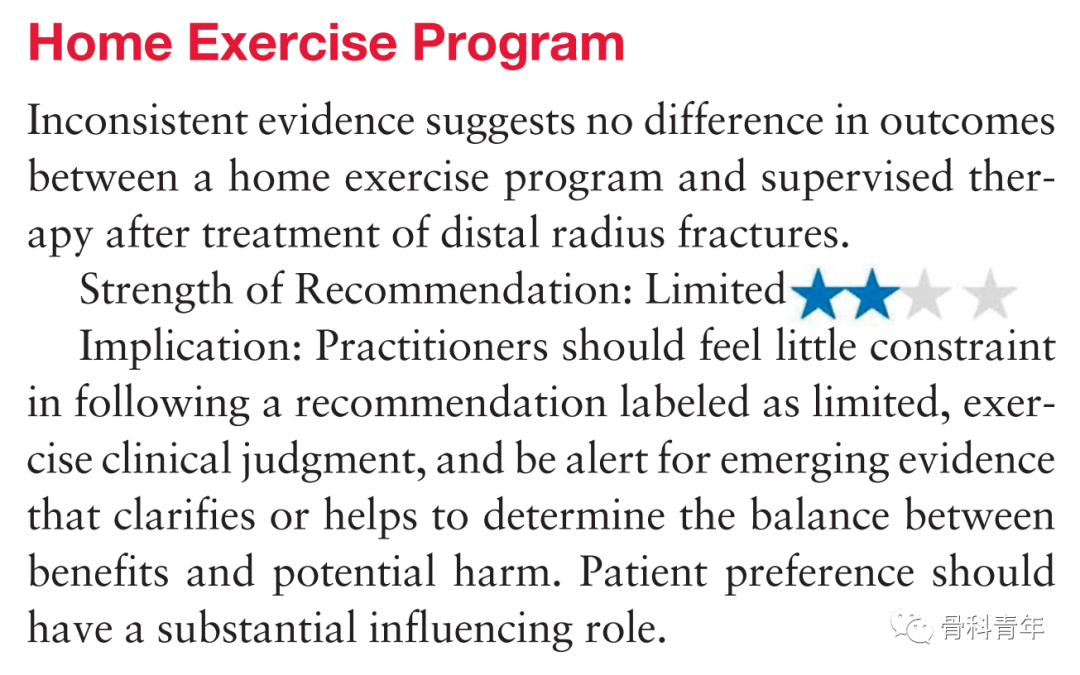
二. 居家锻炼计划(home exercise program)
居家锻炼与治疗师监督下锻炼,结果上无差异。(证据指数:有限)
三. 内固定指征(≤65岁)
对于桡骨短缩大于3mm,背侧成角大于10°,关节面移位或间隙大于2mm患者,手术内固定治疗能够获得更好的影像学及治疗结果。(证据指数:中等)

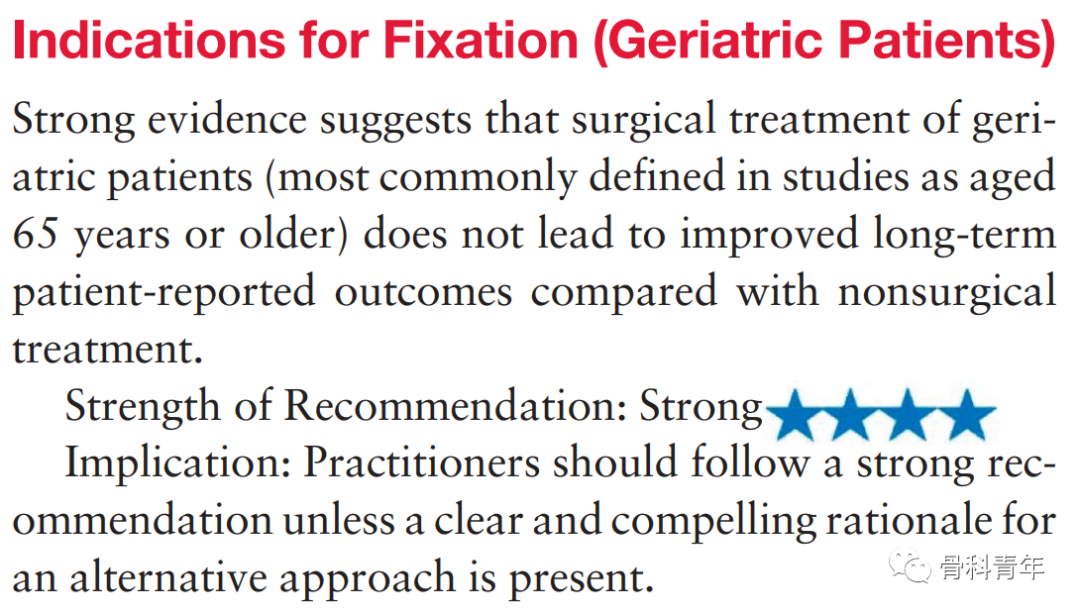
四. 内固定指征(>65岁)
手术治疗及非手术治疗在长远结果来看,无差异。(证据指数:强)
五. 影像学随访(serial radiography)
有限的证据表明,影像学复查的频率,对于治疗结果无差异。(证据指数:有限)
六. 内固定技术(fixation technique)
强有力的证据表明,对于关节内骨折或不稳定的桡骨远端骨折,不同的固定方式在影像学及患者报告的结果来看,无显著差异。尽管掌侧锁定板能进行早期功能康复。(证据指数:强)
七. 阿片类止痛药使用(opioid use)
无证据支持,但是专家组建议对于桡骨远端骨折治疗的患者,应考虑阿片类药物和多模式镇痛管理。(证据指数:专家共识)

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床操作#
121
#AAO#
91
#AAOS#
110
学习了
87
学习了
120
学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习学习
99
Zbc
144
#桡骨远端骨折#
81
#桡骨#
81