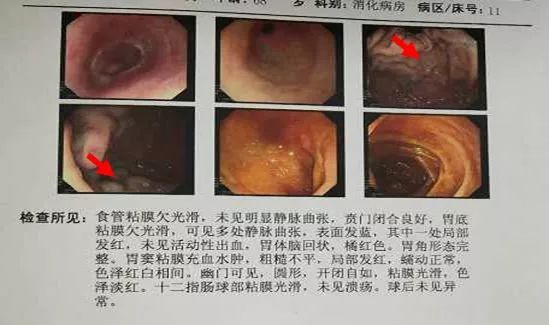
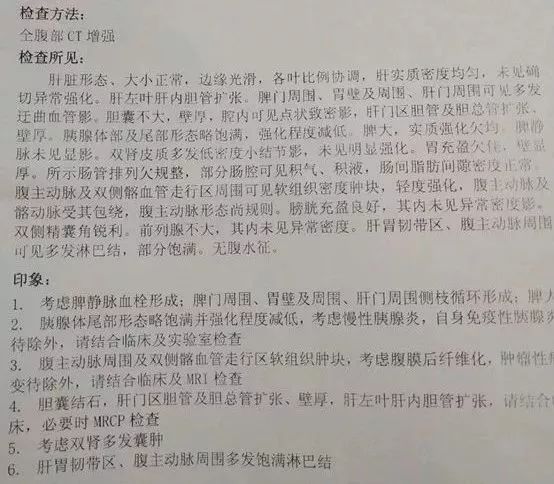
出血原因千千万,此例患者为哪般?
2018-02-06 张云盛 天津医科大学总医院空港医院 医学界消化肝病频道
人体是一个整体的系统,可能罹患多种疾病,作为一个内科医生头脑里应该不单单想到的单学科的某一种疾病。注意详细采集病史,及时完善相关检查,从整体综合分析临床资料,避免孤立、静止地看待某些症状和检查结果,是避免或减少误诊、漏诊的关键。






本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









出血原因的分析.
97
学习了学习了
90
好好好好好好好好
112
了解了解.学习学习
91
学习了
91
学习了很有用不错
43
谢谢分享学习
55
谢谢分享学习了
44
非常好.谢谢分享
52