J Innate Immun:研究发现天然脂质具有超强大的抗炎作用,有望彻底根除炎症性疾病
2018-07-09 细胞 细胞
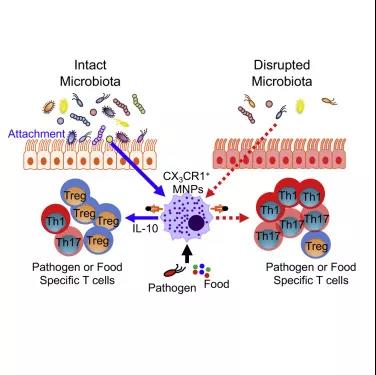
美国国立卫生研究院的研究人员已经发现了一种天然存在的脂质,即一种蜡状的脂肪酸,它被一种致病的细菌用来破坏宿主的免疫反应,增加感染的机会。无意中,他们还发现了一种针对细菌和病毒性疾病的有效炎症疗法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#炎症性疾病#
90
#研究发现#
79
#根除#
77
#Nat#
87
#炎症性#
63
学习了谢谢
129
学习了.谢谢分享
96