Cell Rep:抗体新组合让癌细胞不再隐形
2016-08-03 佚名 生物谷
最近加州大学欧文分校的分子生物学家发现了抗击转移性黑色素瘤的有效方法,他们使用新的创新性免疫治疗方法沉默癌细胞表达的“不要吃我”信号蛋白,使其能够被免疫细胞识别和吞噬。 研究人员发现阻断黑色素瘤细胞表面蛋白CD47(“不要吃我”信号蛋白)能够促进癌细胞被巨噬细胞吞噬。进一步研究表明在阻断CD47的同时靶向另外一个细胞表面蛋白CD271(之前研究发现该蛋白表达在促进黑色素瘤发生的一群癌细胞表面

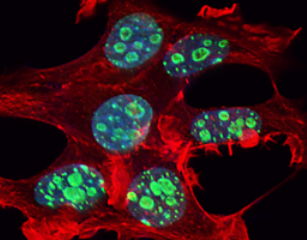
最近加州大学欧文分校的分子生物学家发现了抗击转移性黑色素瘤的有效方法,他们使用新的创新性免疫治疗方法沉默癌细胞表达的“不要吃我”信号蛋白,使其能够被免疫细胞识别和吞噬。
研究人员发现阻断黑色素瘤细胞表面蛋白CD47(“不要吃我”信号蛋白)能够促进癌细胞被巨噬细胞吞噬。进一步研究表明在阻断CD47的同时靶向另外一个细胞表面蛋白CD271(之前研究发现该蛋白表达在促进黑色素瘤发生的一群癌细胞表面),能够导致人源化肿瘤异种抑制小鼠模型(PDX)的肿瘤转移受到完全抑制。相关研究发表在国际学术期刊Cell Reports上。
研究发现细胞表面蛋白CD47在转移性黑色素瘤细胞表面存在过表达,能够帮助细胞避免被免疫系统清除。另一方面CD271之前被证明能够用于标记一个促进肿瘤发生以及癌症转移扩散的黑色素瘤细胞群体。在这项研究中研究人员推测转移性黑色素瘤依赖这两种蛋白的过表达骗过免疫系统进而转移到身体其他部位。
为了验证这一假设,研究人员使用了阻断CD47(激活巨噬细胞的吞噬作用)和CD271(特异性靶向最具侵袭性的黑色素瘤细胞群体)的特异性抗体。他们对移植了人类转移性黑色素瘤的小鼠进行了抗体治疗,发现同时使用两种抗体能够几乎完全清除小鼠所有器官形成的转移灶。他们进一步发现这种治疗作用是由肿瘤微环境发生的巨大变化所介导,能够引起免疫细胞有效地攻击癌细胞。
最后研究人员表示:“还需要进一步研究确定这两种抗体的抗肿瘤转移作用以及应用于人类病人的安全性。但是将这种治疗方法与其他调节免疫系统的治疗方法结合代表了一种新的癌症治疗方法,或将为转移性黑色素瘤病人带来更多获益。癌症免疫治疗带来了癌症治疗的新时代,我们希望我们找到的这种方法能够成为癌症免疫治疗的新组成部分,为更多病人提供有效的治疗效果。”
原始出处
Michael Ngo1, Arum Han1, Anita Lakatos2, Debashis Sahoo3, Stephanie J. Hachey1, Kipp Weiskopf4, Andrew H. Beck5, Irving L. Weissman4, Alexander D. Boiko1.Antibody Therapy Targeting CD47 and CD271 Effectively Suppresses Melanoma Metastasis in Patient-Derived Xenografts.Cell Rep.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
100
#CEL#
83
#癌细胞#
56
继续学习
0
继续关注
93