Arch Phys Med Rehab: 动态平衡训练可提高膝关节炎患者身体功能的初级随机对照实验
2017-09-15 俞陈雨 阳光骨韵
研究发现,膝关节炎(OA)引起的平衡控制能力低下,已经成为老年患者跌倒的重要风险。流行病学报告显示,患有膝关节炎(OA)的老年人的跌倒发生率已经超过50%。目前,针对膝关节炎(OA)患者的动态平衡训练科学证据缺乏,因此本研究通过研究动态平衡训练对膝关节炎(OA)患者疗效,探讨动态平衡训练能否提高膝关节炎(OA)患者动态平衡和身体功能。结论显示,十周的动态平衡训练对于膝关节炎的患者的疼痛、身体功能和
一、背景
研究发现,膝关节炎(OA)引起的平衡控制能力低下,已经成为老年患者跌倒的重要风险。流行病学报告显示,患有膝关节炎(OA)的老年人的跌倒发生率已经超过50%。
目前,针对膝关节炎(OA)患者的动态平衡训练科学证据缺乏,因此本研究通过研究动态平衡训练对膝关节炎(OA)患者疗效,探讨动态平衡训练能否提高膝关节炎(OA)患者动态平衡和身体功能。
二、方法
入选标准:
年龄50- 80岁,影像学证实有胫股关节OA(Kellgren和Lawrence (KL)等级≥2),并且有膝疼痛的患者。
排除标准:
炎症, 膝或髋关节置换术病史, 最近使用糖皮质激素, 膝关节注射, 关节镜手术 (在过去六个月内), 脱离辅助无法步行。神经、肌肉骨骼系统或其他因素影响其下肢运动能力、平衡或最大力量的患者也被排除在外。
三、干预
动态平衡训练组(治疗组):
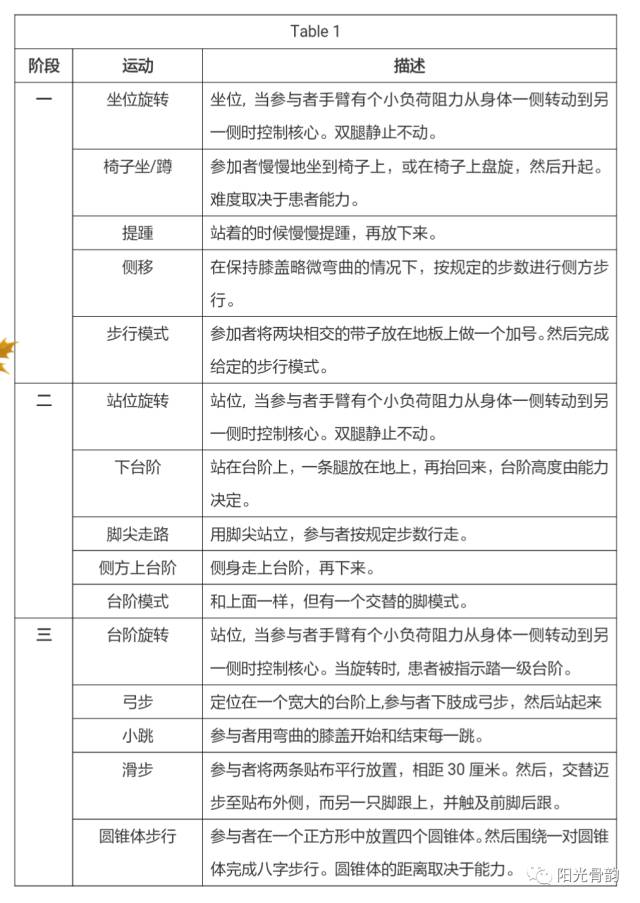
动态平衡训练包括三个阶段的渐进式运动训练,包括强调动态平衡控制、离心下肢肌力和核心稳定性的练习(Table 1)。运动的难度以NRS值测定(0 =无困难;10 =最大困难)。当满足下列条件时,即通过所练习的阶段:1)参与者能够完成每个练习3组,每组12次;2)自觉练习难度低于3 / 10分; 3)当运动学专家认为,该运动已被掌握;4)练习时膝关节疼痛小于6 / 10分。
要求参与者完成所有的练习,每周四次,进行十周。其中六周在监督下进行(在1、2、3、5、7和9周),其他都在家进行训练。
无干预组(对照组):
无干预对照组参加相同的两次测试(基线和随访),参与者被要求保持他们平常的活动水平,并且避免尝试新的治疗方案或药物。
四、疗效测量
1、Community Balance and Mobility Scale(CB&M)
2、Self-reported pain and physical function(WOMAC身体功能量表)
3、Fear of movement(BFMS)
4、肌力(最大离心等速肌力测试:膝屈曲、伸展与踝跖屈肌)
五、结果
40名患者进行基线测试,最终36名完成后续的测试。对照组的任何结果在随访中无明显变化。在运动组,自觉疼痛、身体功能和恐惧运动得到改善。没有其他组内或组间差异。
六、结论
十周的动态平衡训练对于膝关节炎的患者的疼痛、身体功能和运动恐惧感有明显改善,但通过CB&M量化的动态平衡没有变化。
原始出处:
Takacs J, Krowchuk NM, Garland SJ, Carpenter MG, Hunt MA. Dynamic Balance Training Improves Physical Function in Individuals With Knee Osteoarthritis: A Pilot Randomized Controlled Trial. Arch Phys Med Rehabil. August 2017
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#对照#
116
不错的文章.值得一读
128
#关节炎#
61
#膝关节炎#
72
#EHA#
82
#Med#
59
好
92
学习啦!谢谢分享!
93
学习了
90