带膜血管内支架治疗主动脉夹层(图)
2015-12-02 网络 MedSci原创
即往病史: 男性,40岁,高血压病史5年,突发剧烈胸痛5天。UCG:主动脉夹层动脉瘤(Ⅲ型),SCT:主动脉自锁骨下动脉开口至左髂总动脉中段全程夹层。 术前血管造影情况: 主动脉弓分支血管发育畸形,自左至右依次为:无名动脉(该动脉又分出左右颈总动脉)-左锁骨下动脉-右锁骨下动脉。自异常起源的右锁骨下动脉开口以远均为广泛的主动脉夹层,真腔明显变窄,最窄处仅3mm。初始破口位于弓降部
即往病史:
男性,40岁,高血压病史5年,突发剧烈胸痛5天。UCG:主动脉夹层动脉瘤(Ⅲ型),SCT:主动脉自锁骨下动脉开口至左髂总动脉中段全程夹层。
术前血管造影情况:
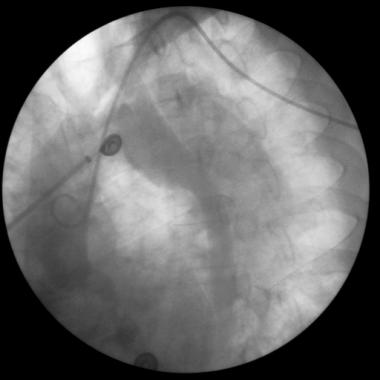
主动脉弓分支血管发育畸形,自左至右依次为:无名动脉(该动脉又分出左右颈总动脉)-左锁骨下动脉-右锁骨下动脉。自异常起源的右锁骨下动脉开口以远均为广泛的主动脉夹层,真腔明显变窄,最窄处仅3mm。初始破口位于弓降部,直径约2cm,可见真假腔之间的异常分流。(图1、2)。远端破口位于左髂总动脉近端,亦可见真假腔内的异常分流(图3)。
手术过程:
(1)穿刺左侧肱动脉,置入5F猪尾巴导管送达主动脉弓部造影可显示主动脉夹层,但未清晰显示破口具体位置及大小,考虑到锁骨下动脉起源异常,故穿刺右侧桡动脉并置入5F猪尾巴导管,造影示破口位于弓降部,直径约2cm,可见血流自破口由真腔高速喷射至假腔(图1)。
(2)初始破口明确后,留置左肱动脉置入猪尾巴导管作定位指示,撤出右桡动脉导管。
(3)1%利多卡因局麻后,手术暴露右侧股动脉,沿股动脉送入300cm的Amplatz Super Stiff导丝,沿导丝送入带膜人造血管内支架,输送器准确定位后,药物将动脉收缩压降至<90mmHg,快速退出输送器,释放人造血管支架。
(4)重复升主动脉造影后,撤出引导钢丝,缝合股动脉。
术后结果/结论:
血管内支架定位及释放满意,主动脉弓分支血管未累及,近端破口堵闭,真腔扩大,假腔缩小,无异常分流,无内漏(图4、5)。随访一年,效果满意,无并发症,复查SCT:血管内支架位置正常,无内漏,假腔大部血栓化。
讨论:
经股动脉置入带膜血管内支架治疗主动脉夹层是近年兴起的一项新技术。其技术要点是:
(1)夹层初始破口的大小、位置一定要明确。
(2)根据破口的位置、大小及与动脉分支的关系选择直径、形状合适的人造血管支架。
(3)防止分支血管受累以免引起脏器缺血,尤其是本例主动脉弓分支血管发育畸形,应特别引起重视。
(4)术中或术后随访一旦发生内漏,应密切观察,及时处理。
带膜血管内支架治疗主动脉夹层
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#支架治疗#
64
#血管内支架#
77
#主动脉#
66
#动脉夹层#
63