European Radiology:MRI在预测乳腺癌患者新辅助化疗病理完全缓解的价值
2022-04-10 shaosai MedSci原创
现阶段,由于影像学上的早期治疗反应是预测乳腺癌pCR的一个指标,因此影像学检查在病情评估中至关重要。
目前,新辅助化疗(NAC)是局部晚期乳腺癌患者的必经之路,可降低分期并手术方式。新辅助化疗取得的生存效果和局部控制与辅助化疗相似。此外,用NAC治疗可以监测治疗反应,其中病理完全反应(pCR)可达24%至37%。一些研究报告称,pCR可作为预测长期预后的替代终点,包括无病生存和总生存,特别是在人类表皮生长因子受体2(HER2)阳性和三阴性亚型中尤为明显。由于影像学上的早期治疗反应是预测pCR的一个指标,因此影像学检查在病情评估中至关重要。磁共振成像(MRI)在评估原发肿瘤范围和对NAC的反应方面比钼靶或超声检查更有优势。
虽然只有少数患者在NAC后获得pCR,但一些临床试验报道了影像学引导下的活检在获得影像学完全反应(rCR)时作为手术替代的潜在效用;因此,预测MRI的pCR变得更加重要。
近日,发表在European Radiology杂志的一项研究根据乳腺癌患者的病理分子亚型,探讨了完成NAC后MRI对pCR的可预测性差异,并研究了究竟哪些MRI征象可以模拟乳腺癌残留,为准确评估预后并制定最佳治疗方案提供了技术支持。
本研究共纳入506名在NAC后接受MRI检查并在2018年1月至12月期间接受手术的乳腺癌患者。由两位乳腺影像学专家将NAC后的MRI结果二分为影像学完全反应(rCR)和无rCR。评估了MRI预测pCR的诊断性能。pCR是根据最终病理报告确定的。肿瘤根据激素受体(HR)和人类表皮生长因子受体(HER)2划分。NAC后MRI上的残余病变分为明显的和隐蔽的,分为结节性或延迟性增强。Pearson's χ2和Wilcoxon秩和检验被用于MRI发现导致的假阴性pCR。
总的pCR率为30.04%。使用MRI预测pCR的总体准确率为76.68%。各亚型的准确率有显著差异(P<0.001),降序排列如下:HR - /HER2 - (85.63%), HR + /HER2 - (82.84%), HR + /HER2 + (69.37%), 和HR - /HER2 + (62.38%)。HR - /HER2 +型的MRI显示预测pCR的假阴性率最高(18.81%)。仅在延迟期观察到的细微残留强化这一征象与假阴性结果相关(76.2%,P = 0.016)。
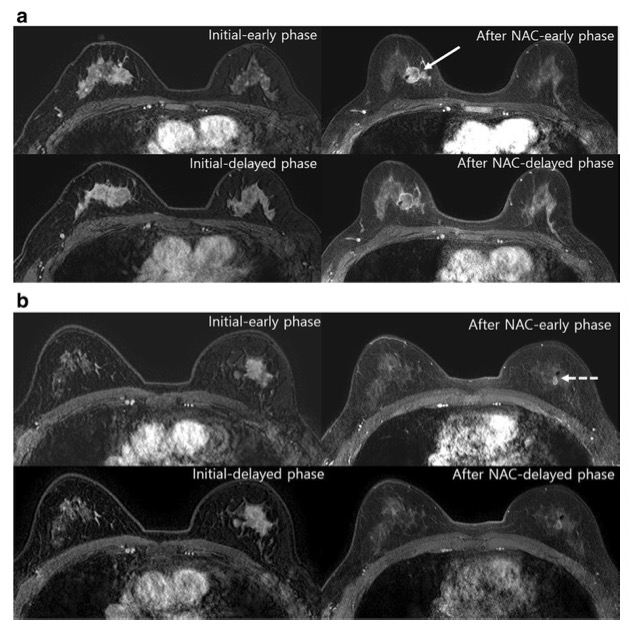
a 50岁女性,患有浸润性导管癌HR-/HER2+亚型的初始MR图像显示,右乳内上象限有一个2.2厘米的不规则强化肿块,有延迟廓清现象。新辅助化疗后的MR图像显示 在同一位置有一个1.8厘米的强化肿块,并伴有延迟廓清。b 54岁女性,患有HR+/HER2+亚型浸润性导管癌,其最初的MR图像显示在左乳的中上象限有一个3.8厘米的不规则强化肿块,有延迟廓清。新辅助化疗后的MR图像显示,在同一位置的标记夹旁有一个0.8厘米的增强性肿块,伴有延迟廓清(早期MR图像中的虚线箭头)。手术后的最终病理报告显示无pCR(ypT1)
总之,HR - /HER2 +亚型乳腺癌NAC后的MRI图像往往与残留的恶性肿瘤具有相似的影像学表现,即使达到pCR也会出现同样的情况。本研究结果表明,当MRI上显示的微弱残余强化且仅在延迟期可看到时,无论分子亚型如何,评估为rCR更加准确。本研究提示,意识到MRI征象对真正pCR的提示可有助于医生在NAC完成后为乳腺癌患者选择更理想的治疗方案。
原文出处:
Jieun Kim,Boo-Kyung Han,Eun Young Ko,et al.Prediction of pathologic complete response on MRI in patients with breast cancer receiving neoadjuvant chemotherapy according to molecular subtypes.DOI:10.1007/s00330-021-08461-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
108
#病理完全缓解#
99
#完全缓解#
144
#新辅助#
119
#乳腺癌患者#
135