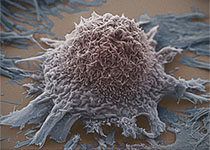
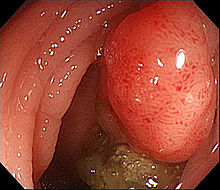
JCEM:雌激素影响结直肠癌进展的机制或与G蛋白偶联受体的增殖有关
2017-09-29 MedSci MedSci原创
背景:尽管目前缺乏精确的分子机制,但雌激素能影响结直肠癌的发生和发展。目的:本研究旨在探讨雌激素代谢的前受体——人类CRC组织、TCGA Coad数据集、体内外的CRC模型研究中的类固醇硫酸酯酶(STS)和17β-羟类固醇脱氢酶的活性,及随后的非基因组雌激素信号,以及确定和哪种雌激素能改变CRC增殖和进展和其治疗的靶向通路。设计、设置、患者和干预:研究人员从绝经后妇女和根据年龄匹配的男性患者中,收
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#G蛋白偶联受体#
34
#G蛋白#
37
#JCE#
27
#JCEM#
30
学习了谢谢分享!!
70
#结直肠#
23
#蛋白偶联#
35
学习了
65