J Infect Dis: 糖尿病和糖尿病前期对抗结核治疗结果的影响
2021-10-25 MedSci原创 MedSci原创
糖尿病 (DM) 已经被世界卫生组织 (WHO) 认可为全球性流行疾病,这种代谢性疾病使活动性结核病 (TB) 的的发生风险增加了三倍。
糖尿病 (DM) 已经被世界卫生组织 (WHO) 认可为全球性流行疾病,这种代谢性疾病使活动性结核病 (TB) 的的发生风险增加了三倍。糖尿病患者血糖控制不佳的时候容易并发多种疾病,而结核是最容易和糖尿病一起发生的一种传染病。有文献报道,糖尿病患者结核感染率是正常人的5-6倍,所以糖尿病患者中结核病还是比较多见的,2019年,全世界约有 400,000 名结核病患者 (PWTB) 被诊断出患有糖尿病。目前尚不清楚糖尿病或糖尿病前期是否会影响结核病患者 (PWTB) 的治疗结果或是会导致死亡风险的增加,因此,本项研究旨在对两者的关系进行进一步分析。

研究人员对2015年至2019年期间参加巴西结核病区域前瞻性观察研究 (RePORT) 的经培养确认的PWTB(n = 643)患者进行了回顾性分析,根据患者基线糖化血红蛋白的血糖状态进行疾病严重程度分层。不利的结核病结果定义为治疗失败或病情恶化、复发或死亡;有利的结果是治愈,Logistic 回归模型评估血糖状态和结果之间的关联。

研究结果显示在这两个队列中,抗TB不良结果与吸烟、非法药物使用和 HIV 感染相关。在巴西结核病例中糖尿病,但不是前驱糖尿病,与不利结果相关(调整后相对风险 [aRR]:2.45,p<0.001),此外,在 RePORT-Brazil队列和 SINAN队列中,糖尿病与高死亡风险(结核病治疗期间)相关 (aRR:2.16, p=0.040) 。
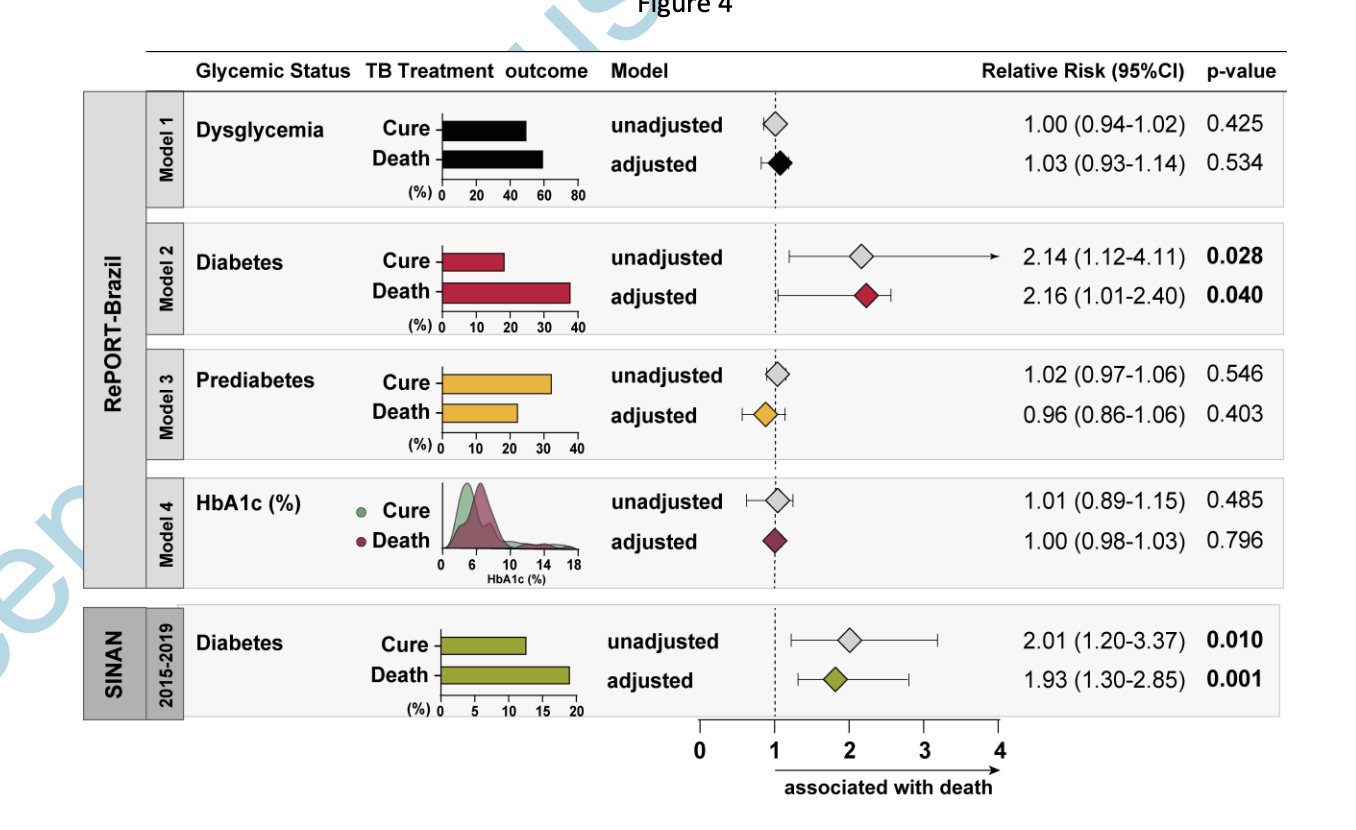
在巴西的肺结核病例中,糖尿病与不良结局和死亡率的风险增加有关。因此,这提醒我们在临床工作中需要采取干预措施来改善糖尿病患者的代谢状态从而改善结核病治疗结果。
原始出处:
María B Arriaga. Et al. The Effect of Diabetes and Prediabetes on Anti-tuberculosis Treatment Outcomes: A Multi-center Prospective Cohort Study.The Journal of Infectious Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dis#
95
已拜读,受益匪浅。
112
#结核#
103
#抗结核#
0
#治疗结果#
0