Invest Ophthalmol Vis Sci:多巴胺缺乏症介导了糖尿病小鼠早期视杆驱动的内部视网膜功能障碍
2018-01-31 cuiguizhong MedSci原创
美国佐治亚州亚特兰大Emory大学眼科学系的Kim MK近日在Invest Ophthalmol Vis Sci发表,他们发现,早期糖尿病的内部视网膜功能障碍是由rod信号途径功能紊乱和多巴胺(DA)缺陷介导的。振荡电位(OPs)延迟可用于鉴定糖尿病视网膜病变中最早的功能缺陷。
美国佐治亚州亚特兰大Emory大学眼科学系的Kim MK近日在Invest Ophthalmol Vis Sci发表,他们发现,早期糖尿病的内部视网膜功能障碍是由rod信号途径功能紊乱和多巴胺(DA)缺陷介导的。振荡电位(OPs)延迟可用于鉴定糖尿病视网膜病变中最早的功能缺陷。
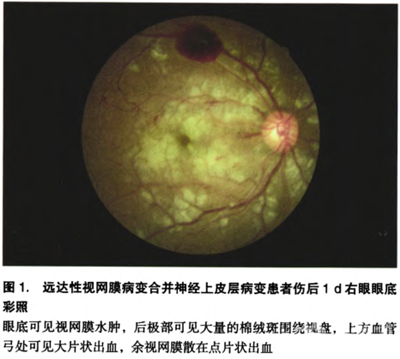
在血管病变出现之前,通过视网膜电图(ERG)可以发现糖尿病患者的视网膜异常,这为糖尿病患者的视力丧失提供了潜在的生物标志物。此前,作者的研究发现,在糖尿病模型的啮齿动物中,视网膜中多巴胺(DA)水平下降导致早期视觉和视网膜功能障碍。在这项研究中,他们检查了振荡电位(OPs)是否可以作为检测早期内部视网膜功能障碍的潜在标志物。

在用链脲佐菌素诱导糖尿病发生后3周、4周和5周,用暗适应的视网膜电图(ERG)来检测视网膜功能。对电响应进行分析,并分析与视网膜多巴胺(DA)水平之间的相关性。使用L-3,4-二羟基苯丙氨酸(L-DOPA)处理的小鼠和视网膜特异性酪氨酸羟化酶(Th)敲除小鼠(rTHKO),在两种小鼠模型上分别评估恢复全身DA水平或从糖尿病小鼠的视网膜中降低DA对振荡电位(OPs)的影响。
结果他们发现,与对照动物相比,糖尿病模型动物响应昏暗但不明亮的闪光刺激,使OP显着延迟。 L-DOPA治疗恢复了糖尿病小鼠OP延迟时间。与具有正常视网膜酪氨酸羟化酶(Th)的糖尿病小鼠相比,糖尿病rTHKO小鼠进一步延迟了OP。视网膜DA水平的降低与由rod信号通路介导的OP延迟增加显着相关。
因此,这项研究数据表明,早期糖尿病的内部视网膜功能障碍是由rod信号途径功能紊乱和多巴胺(DA)缺陷介导的。振荡电位(OPs)延迟可用于鉴定糖尿病视网膜病变中最早的功能缺陷,并确定DA治疗的早期治疗窗口,可防止进行性视力丧失。
原文出处:
Kim, M.K., et al., Dopamine Deficiency Mediates Early Rod-Driven Inner Retinal Dysfunction in Diabetic Mice. Invest Ophthalmol Vis Sci, 2018. 59(1): p. 572-581.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EST#
58
#视网膜#
61
#功能障碍#
60
#THA#
59
学习了新知识
78
了解了解.继续关注
85
学习学习学习
92
好好好好好好好好
89
学习了
96
非常好.谢谢分享
48