JACC:PCI术后替卡格雷和双重抗凝治疗的比较
2019-10-30 不详 MedSci原创
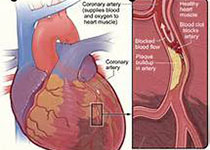
GLOBAL LEADERS临床试验将15991名接受经皮冠脉介入治疗患者随机分成1个月双重抗血小板治疗(DAPT)后接受23个月的替卡格雷治疗和传统的12个月DAPT治疗后12个月阿司匹林治疗组。主要有效终点事件是全因死亡、非致死性心梗、非致死性卒中或紧急靶血管血运再生。本研究结果发现,试验组和传统治疗组患者2年后的主要有效终点事件发生率分别是7.14%和8.41%(RR: 0.85; 95%
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
89
#PCI术#
91
#ACC#
85
#替卡格雷#
93
#PCI术后#
89
学习一下
153
认真学习了,谢谢!
141
学习了,谢谢分享
117