Blood:无亲缘关系的脐带血与HLA单倍体相合供体骨髓移植的预后对比
2020-09-06 QQY MedSci原创
骨髓移植是多种血液病的唯一一种可治愈的疗法,但移植供体的选择困难成为制约移植的主要障碍。两个关于移植无亲缘关系的脐带血或来自HLA-单倍体相合供体的骨髓移植的平行二期试验对这两种供体来源进行了直接对比
2012年6月-2018年6月,共有368位18-70岁的化疗敏感的淋巴瘤或处于缓解期的白血病患者,被随机分至脐带血(n=186)或单倍体相合(n=182)移植。对这两种供体类型,减强度调节包括全身放疗联合环磷酰胺和氟达拉滨化疗。脐带血移植后的移植物抗宿主病预防疗法是环孢素和吗替麦考酚酯,单倍体相合移植后的预防疗法是环磷酰胺、他克莫司和吗替麦考酚酯。主要终点是2年无进展存活率。
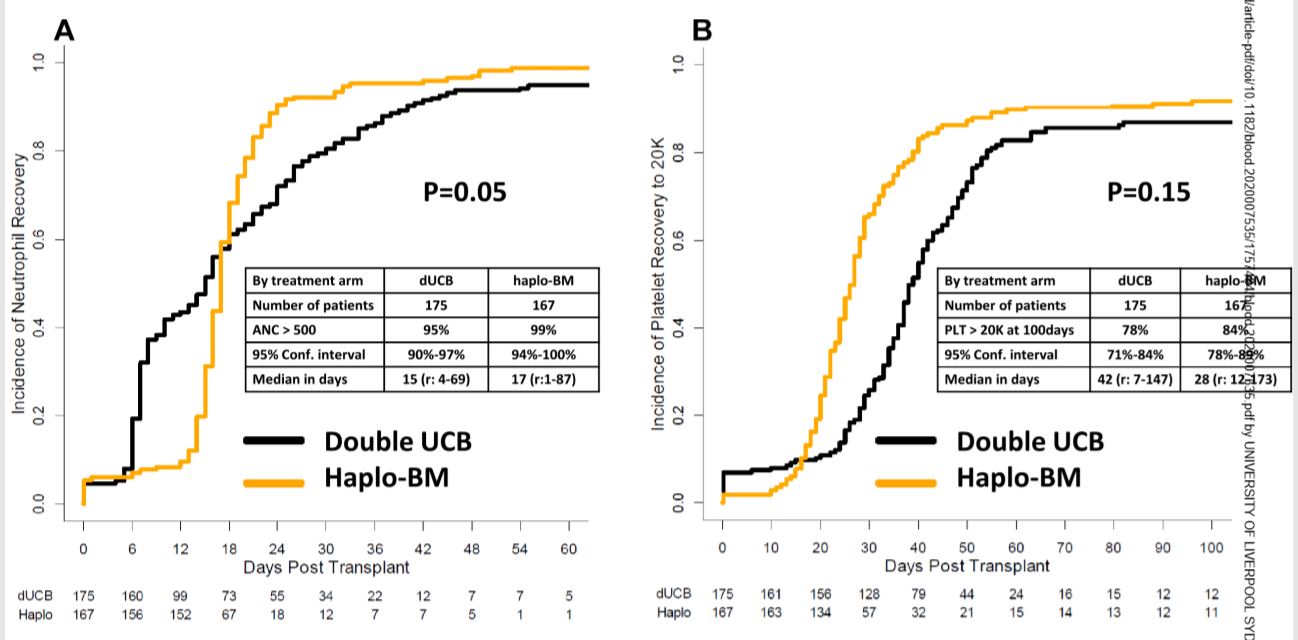
随机分组时,治疗组有相似的年龄、性别、自我报告的种族、表现状况、疾病和疾病状况。脐带血和单倍体相合移植后的2年无进展存活率分别是35%(95% CI 28-42%)和41%(34-48%,p=0.41)。预先指定的次要终点分析显示,脐带血移植后的2年非复发死亡率为18% (95% CI 13-24%),高于单倍体相合移植术后的11% (95% CI 6-16%,p=0.04)。脐带血移植和单倍体相合移植术后的2年总体存活率分别为46% (95% CI 38-53)和57% (49-64%,p=0.04)。
总体上,该试验两种移植来源的主要终点、2年无进展存活率均无明显统计学差异。虽然两种供体来源都扩大了低强度移植的可获得性,但对包括总生存率在内的次要终点分析均提示,单倍体相合供体来源的骨髓移植的预后可能更好一些。
原始出处:
Ephraim J Fuchs,et al. Double unrelated umbilical cord blood versus HLA-haploidentical bone marrow transplantation (BMT CTN 1101). Blood. August 31,2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#供体#
119
#脐带血#
115
#HLA#
140
#脐带#
94
学习
154