Eur Heart J:既往冠状动脉搭桥术的非ST段抬高急性冠状动脉综合征患者有创与保守治疗比较
2024-06-02 MedSci原创 MedSci原创 发表于上海
这项荟萃分析证实了NSTE-ACS患者接受保守治疗方法相比,常规有创策略没有任何益处。这些发现应该在足够有力的随机对照试验中进行验证。
对于非ST段抬高急性冠状动脉综合征(NSTE-ACS)高危患者,建议采用常规有创性治疗策略。这是基于多个随机对照试验(RCTs)的结果,这些试验比较了常规有创与保守或选择性有创策略。冠状动脉旁路移植术(CABG)的患者约占NSTE-ACS患者的10%,并且由于他们年龄较大,合并症较多,与没有CABG的患者相比死亡率增加,因此属于高风险亚组。观察性数据一致报道,既往冠脉搭桥的ACS患者较少接受血管造影或随后的经皮冠状动脉介入治疗(PCI)。值得注意的是,既往CABG患者被排除在NSTE-ACS指南的一些关键试验之外,因此常规有创治疗策略的益处在该组中不太确定。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员对随机对照试验(RCT)进行系统评价和荟萃分析。首先,研究人员对PubMed、EMBASE、Cochrane和ClinicalTrials.gov进行了全面地检索。符合条件的研究是在NSTE-ACS患者(包括既往冠脉搭桥患者)中进行常规有创与保守或选择性有创策略的随机对照试验。如果以前未发表,则从每个试验的作者处收集汇总数据。评估的结局包括全因死亡率、心脏死亡率、心肌梗死和心脏相关住院。采用随机效应模型,计算95%置信区间的风险比(RR)。
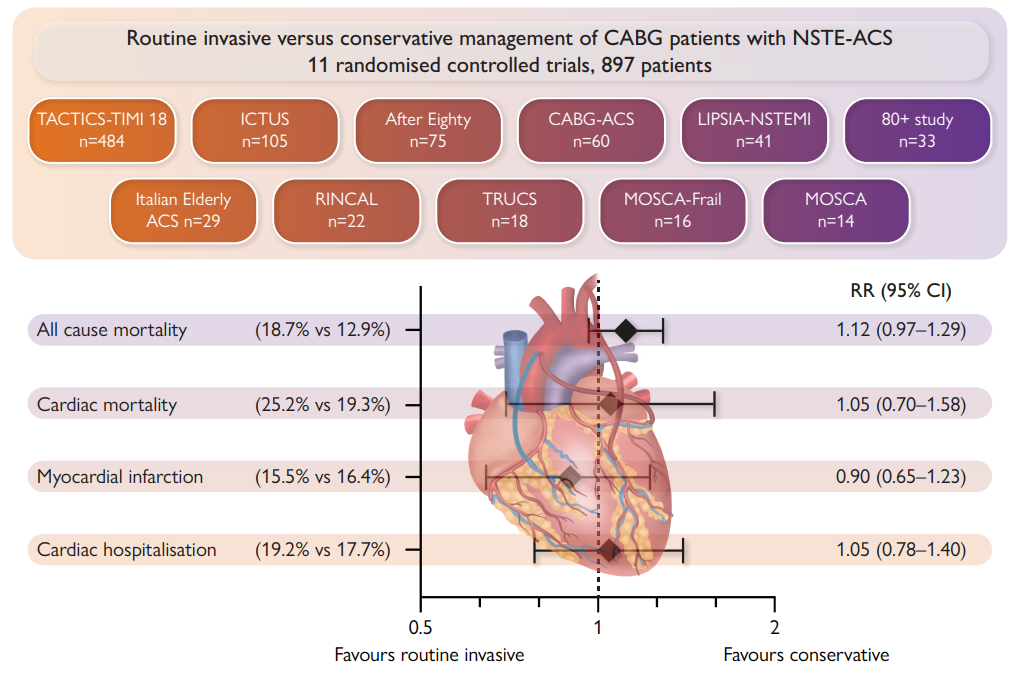
汇总数据来自11项随机对照试验,包括先前未发表的9项试验的亚组结果,其中包括897例既往CABG患者(477例常规有创性,420例保守/选择性有创性),加权平均随访2.0年(范围为0.5-10)。常规有创策略不能降低全因死亡率(RR为1.12, 95%CI为0.97-1.29)、心脏死亡率(RR为1.05, 95%CI为0.70-1.58)、心肌梗死(RR为0.90, 95%CI为0.65-1.23)或心脏相关住院(RR为1.05, 95%CI为0.78-1.40)。
由此可见,这项荟萃分析证实了NSTE-ACS患者接受保守治疗方法相比,常规有创策略没有任何益处。这些发现应该在足够有力的随机对照试验中进行验证。
原始出处:
Matthew Kelham,et al.Non-ST-elevation acute coronary syndromes with previous coronary artery bypass grafting: a meta-analysis of invasive vs. conservative management.European Heart Journal.2024.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehae245/7684162
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享
21
#非ST段抬高急性冠状动脉综合征# #既往冠状动脉搭桥术#
30
谢谢分享
30
学习了,谢谢分享
24
很有用
26