JAHA:脂蛋白(a)水平与房颤和缺血性卒中的关系!
2017-12-16 xing.T MedSci原创
由此可见,Lp(a)水平与AF发生无关,Lp(a)水平与缺血性卒中风险增加有关,主要是在AF患者中,而在无AF患者中则无关。
脂蛋白(a)(Lp[a])会促进动脉粥样硬化和促进血栓形成,与冠心病以及其他心血管疾病的发生有关。在房颤(AF)患者中,Lp(a)与AF发生和缺血性卒中之间的相关性仍有待阐明。
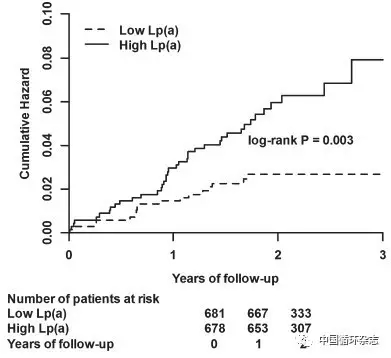
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,在社区为基础的ARIC(社区动脉粥样硬化风险)研究队列中,研究人员在第4次随访时(1996年-1998年)通过试剂盒测量了受试者的Lp(a)水平,并采用多变量调整的Cox模型来比较不同Lp(a)水平的AF和缺血性卒中风险。首先,研究人员评估了9908名在基线时没有AF的参与者AF的发生情况。通过研究随访时的心电图、医院国际疾病统计分类第九版修订(ICD-9)代码和死亡证明中来证实AF。然后研究人员对10127名基线无卒中患者的缺血性卒中进行了评估。通过年度电话、医院ICD 9修订码和死亡证明来确定卒中。
参与者基线年龄为62.7±5.6岁。中位数的Lp(a)水平为13.3 mg/dL(间距范围为5.2-39.7mg/dL)。AF和卒中的中位随访时间分别为13.9年和15.8年。比较那些Lp(a)≥50与Lp(a)<10 mg/dL的参与者,研究人员发现Lp(a)与AF事件发生无关(风险比为0.98;95%可信区间为0.82-1.17)。在没有AF的参与者中,高Lp(a)与卒中风险相对增加42%有关(风险比为1.42,95%可信区间为1.07-1.90),但在AF患者中则无关(风险比为1.06,95%可信区间为0.70-1.61,AF相互作用P=0.25)。种族或性别无相互作用。心源性卒中的亚型之间未发现相关性。
由此可见,Lp(a)水平与AF发生无关,Lp(a)水平与缺血性卒中风险增加有关,主要是在AF患者中,而在无AF患者中则无关。
原始出处:
Konstantinos N. Aronis,et al. Associations of Lipoprotein(a) Levels With Incident Atrial Fibrillation and Ischemic Stroke: The ARIC (Atherosclerosis Risk in Communities) Study.JAHA.2017. https://doi.org/10.1161/JAHA.117.007372
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#缺血性卒#
64
脂蛋白a会促进动脉硬化.
87
学习了谢谢分享!!
93
#缺血性#
70
学习了.谢谢分享!
102
#AHA#
50
#脂蛋白#
67