JAMA Neurology: SARS-CoV-2感染可能引起免疫性肌病
2021-06-13 MedSci原创 MedSci原创
大多数COVID-19重症患者表现出从轻微到严重的肌炎症状。骨骼肌的炎症与疾病的持续时间有关,并且比心脏炎症更明显。SARS-CoV-2可能与一种感染后免疫介导的肌病有关。
有临床研究报道COVID-19患者有肌痛、肌酸激酶水平升高和持续肌无力等症状。SARS-CoV-2感染是否有covid -19相关肌病,这种疾病是病毒还病毒后现象?目前并无研究报道。从轻度肌炎到致死性横纹肌溶解症的肌病与许多不同的病毒有关。然而,临床上怀疑为病毒相关肌炎的病例很少进行肌肉活检。因此,到目前为止,只有病例报告和小系列提供一些组织病理学的见解。
近期JAMA Neurology杂志发文报道了来自严重COVID-19死亡个体的骨骼肌样本的组织病理学、病毒学、免疫学和超微结构研究结果,并将其与非COVID-19危重患者的骨骼肌样本进行比较。
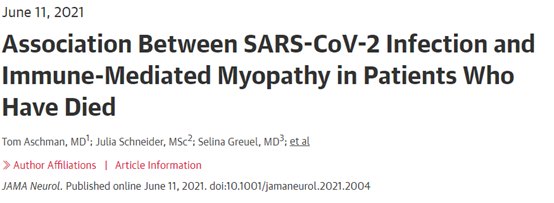
这个病例对照尸检研究包括2020年3月至2021年2月期间死亡并进行尸检的COVID-19或其他重大疾病患者。随机选取知情同意解剖且解剖间隔不超过6天的个体。将SARS-CoV-2PCR检测结果阳性且有COVID-19临床特征的个体与PCR检测结果呈阴性且无COVID-19临床特征的个体进行比较。骨骼肌组织的炎症通过定量免疫细胞浸润、肌膜上I类和II类抗原的主要组织相容性复合体(MHC)的表达,以及从病理缺失到最显著的病理的视觉模拟量表的盲评来评估。心肌炎症通过免疫细胞浸润定量评估。
COVID-19患者43例(年龄中位数[四分位数范围],72[16]岁;31名男性(72%)和11名非COVID-19患者(年龄中位数[四分位数范围],71[5]岁;其中包括7名男性(64%)。
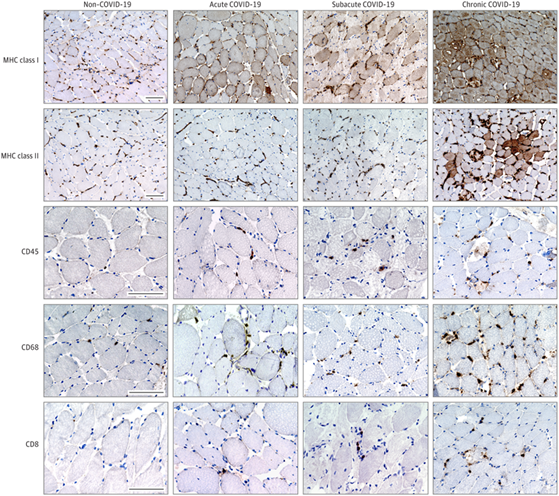
COVID-19死亡患者的骨骼肌样本显示更高的总体病理评分(平均[SD], 3.4 [1.8] vs 1.5 [1.0];95%可信区间,0 - 3;P<0.001)和更高的炎症评分(平均[SD],3.5 [2.1] vs 1.0 [0.6];95%可信区间,0 - 4;P <0.001)。42例COVID-19患者标本中23例(55%)肌纤维膜上MHC I类抗原表达相关,42例COVID-19患者标本中7例(17%)MHC II类抗原表达上调,但在对照组中均未发现。自然杀伤细胞数量增加(中位数[四分位数范围],每10个高倍镜视野8 [8]vs 3[4]个细胞;95% CI,每10个高倍镜视野1-10个细胞;P<0.001)。
与COVID-19患者相比,非COVID-19危重患者骨骼肌炎症变化
免疫组化显示自然杀伤细胞,未检测到SARS-CoV-2刺突蛋白
骨骼肌的炎症特征多于心肌,且慢性COVID-19患者中炎症最为明显。在部分肌肉标本中,通过PCR反应检测到SARS-CoV-2 RNA,但免疫组化和电子显微镜未发现直接病毒感染肌纤维的证据。
在该病例对照研究中,大多数COVID-19重症患者表现出从轻微到严重的肌炎症状。骨骼肌的炎症与疾病的持续时间有关,并且比心脏炎症更明显。大多数骨骼肌和心肌的病毒载量检测为低或阴性,这可能归因于循环病毒RNA,而不是真正的肌细胞感染。这表明SARS-CoV-2可能与一种感染后免疫介导的肌病有关。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#SARS-CoV#
0
#Neurol#
60
#SARS#
54
#肌病#
54
非常好
84
学习
74
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
60