Eur Urol:前列腺根治性切除术后局部复发患者的抢救手术
2020-12-31 AlexYang MedSci原创
自前列腺特异性膜抗原(PSMA)正电子发射断层扫描(PET)成像技术问世以来,人们可以准确划分根治性前列腺切除术(RP)后的孤立性局部复发。
自前列腺特异性膜抗原(PSMA)正电子发射断层扫描(PET)成像技术问世以来,人们可以准确划分根治性前列腺切除术(RP)后的孤立性局部复发。
最近,有研究人员描述和评估了精囊床局部复发患者抢救性手术后的外科技术、生化响应和无治疗生存(TFS)情况。研究人员回顾性评估了两个中心的40名接受开放性抢救手术治疗的患者(11/2014-02/2020)。所有患者在RP后出现生化复发(BCR),且PSMA PET成像时出现单一的局部复发。33名(82.5%)患者先前接受过挽救性放疗。研究结果表明,抢救性手术前,PSA中位数为0.9 ng/ml(四分位数范围[IQR]:0.5-1.7 ng/ml)。术后,PSA中位数最低值为0.1 ng/ml(IQR:0-0.4 ng/ml)。在31名(77.5%)患者中观察到了cBR。在中位数为24.4个月的随访期间,22名(55.0%)患者出现BCR,12名(30.0%)患者接受了进一步治疗。在1年的随访中,无BCR生存率为62.2%,TFS率为88.3%。研究人员观察到3例(7.5%)Clavien-Dindo III级并发症。研究的主要局限性是回顾性设计、随访时间短以及缺乏对照组。
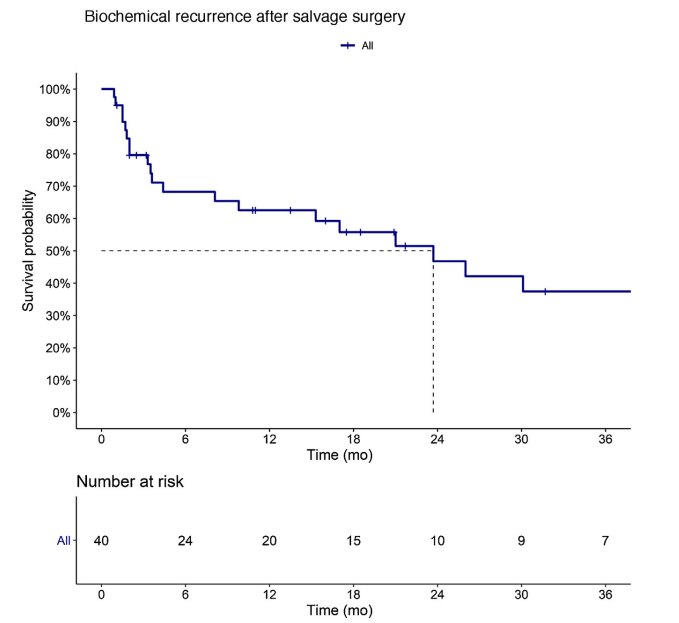
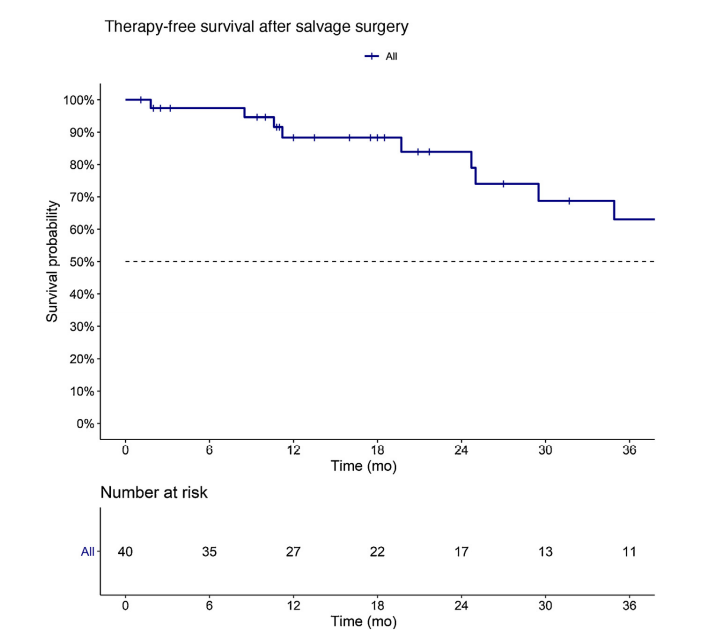
最后,研究人员指出,精囊床内局部复发的抢救性手术是可行的。在选择的、局部复发的患者中,它可能是一个延长无BCR生存期和增加TFS的机会。研究人员也指出需要进一步的研究来证实上述发现。
原始出处:
Sophie Knipper, Luigi Ascalone, Benjamin Ziegler et al. Salvage Surgery in Patients with Local Recurrence After Radical Prostatectomy. Eur Urol. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
36
#局部复发#
50
学习了
83
#局部#
40
#抢救#
48
#根治性切除术#
40
#根治#
35