Nature:免疫疗法关键靶点PD-L1竟有不为人知的“帮手”
2017-08-18 Chen 生物探索
PD-1/PD-L1无疑是癌症免疫治疗领域最热门的一对靶点。8月16日,在线发表于Nature杂志上的两篇论文同时发现了调节PD-L1的一个先前未知的分子——CMTM6。有趣的是,两个科学家团队利用了完全不同的方法得出了相同的结论。魔剪CRISPR又在其中一篇论文中立了一功。
PD-1/PD-L1无疑是癌症免疫治疗领域最热门的一对靶点。8月16日,在线发表于Nature杂志上的两篇论文同时发现了调节PD-L1的一个先前未知的分子——CMTM6。有趣的是,两个科学家团队利用了完全不同的方法得出了相同的结论。魔剪CRISPR又在其中一篇论文中立了一功。

Checkpoint inhibitors (blue) and T-cells (brown) in the bloodstream. Immunotherapy with checkpoint inhibitors is currently used by patients with for example melanoma, lung cancer and renal cancer. Credit: The Netherlands Cancer Institute
在癌症免疫疗法领域,PD-1/PD-L1无疑是最热门的一对靶点。目前,美国FDA已经批准了2款PD-1抗体(Opdivo和Keytruda)以及3款PD-L1抗体(Tecentriq、Bavencio、Imfinzi)上市,用于治疗包括黑色素瘤、非小细胞肺癌、肾细胞癌、经典型霍奇金淋巴瘤、头颈癌、膀胱癌、结直肠癌等近十种癌症。
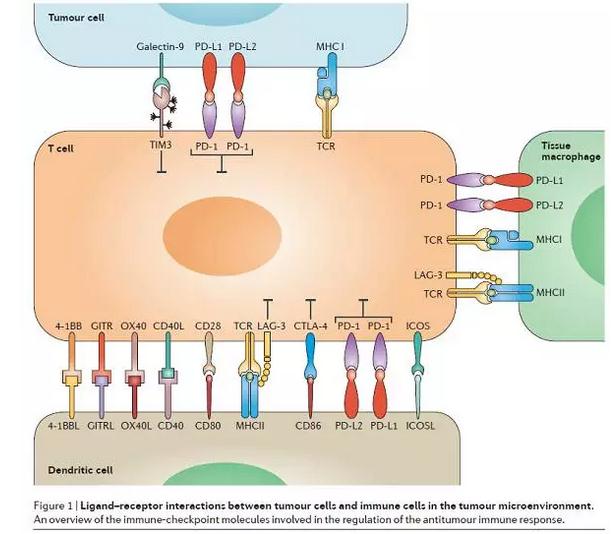
图片来源:Nature Reviews Clinical Oncology
1揭秘PD-L1不为人知的“同盟军”
然而,尽管已经有癌症患者能够获益于靶向PD-1/PD-L1的药物,但是与这些靶点相关的大部分信息仍不为人知,比如,为什么一些癌症比其它的癌症携带的这类分子更多?
8月16日,发表在Nature杂志上题为“Identification of CMTM6 and CMTM4 as PD-L1 protein regulators”的论文中,来自荷兰癌症研究所的科学家们发现了一个重要的线索,揭秘了PD-L1分子一个先前未知的“伙伴”——CMTM6。
具体来说,利用单倍体遗传筛选,研究鉴定出3型跨膜蛋白CMTM6的新功能——作为PD-L1蛋白的调节器。在所有测试的人类肿瘤细胞类型以及人类树突状细胞中,干扰CMTM6的表达都导致了PD-L1表达受损。此外,通过在CMTM6缺陷细胞(CMTM6-deficient cell)中的单倍体遗传修饰筛选以及遗传互补试验,研究人员证明,CMTM6最“亲密”的家族成员CMTM4共享了这一功能。同时,研究发现,CMTM6存在于细胞表面,降低了PD-L1蛋白的泛素化,增加了它的半衰期。此外,与其对PD-L1蛋白的调节作用相一致,CMTM6增强了表达PD-L1的肿瘤细胞抑制T细胞的能力。
该研究的共同通讯作者Ton N. M. Schumacher教授说:“我们一直认为,PD-L1在癌细胞表面是一个‘孤独者’,但我们的发现表明,事实上,它结合了另一种被称为CMTM6的蛋白。CMTM6稳固了PD-L1,从而增加了癌细胞抑制免疫响应的能力。”
科学家们认为,这一研究除了进一步理解了PD-L1检查点的作用机理外,也揭示了癌症免疫疗法的新靶点。Schumacher教授说:“你可以想象,阻断CMTM6能够重新激活免疫细胞的抗癌作用,就像现在的PD-L1阻断剂能做到的那样。此外,同时阻断这两个分子甚至可能产生更加好的抗癌作用。这是我们迫切需要检测的东西。”
此外,这一新发现的PD-L1的“伙伴分子”还有可能作为生物标志物,帮助临床医生预测是否患者能够获益于检查点抑制剂这类免疫疗法。研究人员现在正在用PD-L1抗体治疗的患者中调查这种可能性。
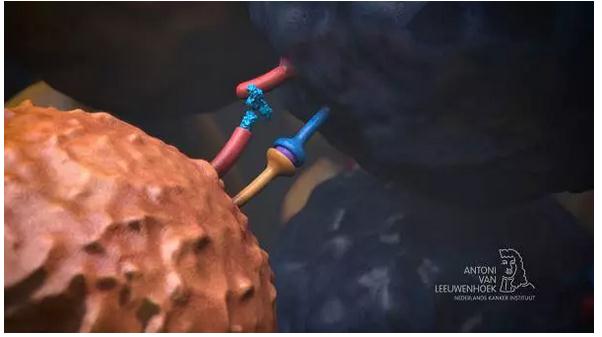
The checkpoint inhibitor (blue) prevents binding of the checkpoint by the cancer cell so the T-cell can kill the cancer cell. Credit: The Netherlands Cancer Institute
2同日另一篇Nature:方法不同,结论相同
有趣的是,在同日发表的另一篇Nature论文中(题目:CMTM6 maintains the expression of PD-L1 and regulates anti-tumour immunity),来自澳大利亚和英国的一个科学家团队发现了关于CMTM6的相同结果。值得一提的是,基因编辑工具CRISPR参与这一重要结论的发现。
具体来说,在这篇论文中,科学家们利用全基因组CRISPR–Cas9筛选发现,在广泛的癌细胞中,CMTM6是PD-L1的关键调节因子。研究称,CMTM6与PD-L1共定位(co-localizes)在质膜和循环核内体(endosomes)上。在这里,CMTM6能够阻止PD-L1成为溶酶体介导的降解作用的目标。
同时,通过一个定量途径对整个质膜蛋白质组进行分析发现,CMTM6表现出了对PD-L1的特异性。删除CMTM6会降低PD-L1,但不影响MHC I类分子在细胞表面的表达。此外,删除CMTM6会在体内和体外通过降低PD-L1显著减轻对肿瘤特异性T细胞活性的抑制。
与荷兰癌症研究所的研究结论一致,该研究称,这些发现为PD-L1调节生物学提供了新的见解,鉴定出了这一关键免疫检查点先前未被发现的主要调节器,指出了克服癌细胞免疫逃逸的潜在治疗靶点。
Schumacher教授说:“我们使用了不同的方法来发现同样的结果。我想,我们都非常高兴看到这种独立的验证。”
原始出处:
1)Mezzadra R, Sun C, Jae LT,et al.Identification of CMTM6 and CMTM4 as PD-L1 protein regulators.Nature. 2017 Aug 16. doi: 10.1038/nature23669.
2)Burr ML, Sparbier CE, Chan YC,et al.CMTM6 maintains the expression of PD-L1 and regulates anti-tumour immunity.Nature. 2017 Aug 16. doi: 10.1038/nature23643.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
65
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
110
#PD-L1#
66
太巧了!但是这也是互相印证对方的理论
106