JAMA Oncol:西妥昔单抗对接受紫杉醇、顺铂及放疗的食管癌患者的影响
2017-07-07 zhangfan MedSci原创
对于食管癌患者,在现有的放化疗基础上联合西妥昔单抗不能提高总生存率。目前EGFR靶向药物对食道癌患者收益不大,强调了生物标志物检测在食管癌治疗中的必要性
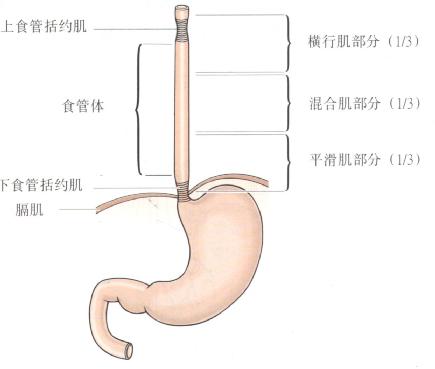
对于非手术治疗的食管癌患者,表皮生长因子受体(EGFR)抑制剂在放化疗策略中的作用尚不清楚。近日研究人员评估了西妥昔单抗对于同步放化疗食管癌患者的治疗作用。美国国立癌症研究所(NCI)发起这项多中心、III期随机临床试验,招募了344名食管活检证实的食管癌患者,研究2008-13年进行。患者每周注射顺铂(50mg/m2),紫杉醇(25mg/m2),每日接受放疗,总剂量50.4Gy(1.8Gy每次),患者随机每周注射西妥昔单抗(第一天400mg/m2,之后每周250 mg/m2)或安慰剂。主要终点是总生存率。研究招募了344名患者,其中328名患者符合数据评估要求(试验组159人,对照组169人)。所有患者肿瘤特征匹配良好:T3或T4阶段263人(80%),N1患者215人(66%),腹腔淋巴结受累62人(19%)。3-5级的治疗相关不良事件发生病例:试验组,71 例(46%), 35 例(23%), 6例 (4%);对照组,83 例(50%), 28 例(17%), 2例 (1%)。试验组的临床完全应答患者81例(56%),对照组92 例(58%),无显著差异。所有患者的中位随访时间为
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#西妥昔#
58
#Oncol#
64
#铂#
58
很好,不错,以后会多学习
100
#食管癌患者#
60
#食管#
56
很好,不错,以后会多学习
98