Stroke:CTA动脉闭塞类型决定了支架取栓成功率
2017-12-03 杨中华 脑血管病及重症文献导读
支架回收(Stent retriever,SR)血栓切除术是急性颅内大动脉闭塞主要的血管内治疗(EVT)方法。然而,SR无效者大约为20%。如果手术前能够预测SR是否成功,那么我们可以采取更有效的EVT方法。
支架回收(Stent retriever,SR)血栓切除术是急性颅内大动脉闭塞主要的血管内治疗(EVT)方法。然而,SR无效者大约为20%。如果手术前能够预测SR是否成功,那么我们可以采取更有效的EVT方法。
急性颅内大动脉闭塞的病理机制是SR成功的主要因素。一般认为,SR对非心源性颅内大动脉闭塞的作用较小,比如颅内大动脉粥样硬化性狭窄,在亚洲人群中颅内大动脉粥样硬化占急性颅内大动脉闭塞的15-20%。人们采取了不同的方法判断颅内大动脉闭塞的病理机制,比如动脉高密度征或磁敏感血管征、随访影像发现恒定的局部狭窄、取出血栓的组织学检查以及超急性期过后进行广泛地心脏学检查等。然而,急性颅内大动脉闭塞的血管内治疗具有时间敏感性,手术前推测病理机制的方法是有限的。
一项最近的研究显示,血管造影的闭塞类型(DSA定义闭塞类型)与发病的病理机制有关,时SR成功的强预测因子。为了优化EVT治疗方法,于开始治疗前而不是治疗后判断闭塞类型将是有帮助的。选择最佳EVT方法有助于成功再通,同时能够缩短穿刺到再通的时间。
2017年10月来自韩国的Jang-Hyun Baek等在Stroke上发表了他们的研究结果,目的在于探讨SR成功的手术前预测因素,他们假设:1.CTA能够判断闭塞类型;2.CTA闭塞类型和DSA闭塞类型一样能够预测SR成功。
该研究回顾分析了进行过CTA检查并且进行了血管内治疗的连续颅内大动脉闭塞性卒中患者。研究者把CTA动脉闭塞类型分为干型闭塞或分支部位闭塞,并与血管内治疗期间的DSA闭塞类型相比较。研究者还评价了3项手术前的检查所见包括CTA闭塞类型、房颤和动脉高密度征,这三项能够推测闭塞的病理机制比如栓塞还是非栓塞,并且具备迅速和容易评价的特点。研究者评价了这三项手术前检查所见与SR成功、卒中危险因素和实验室结果之间的关系。
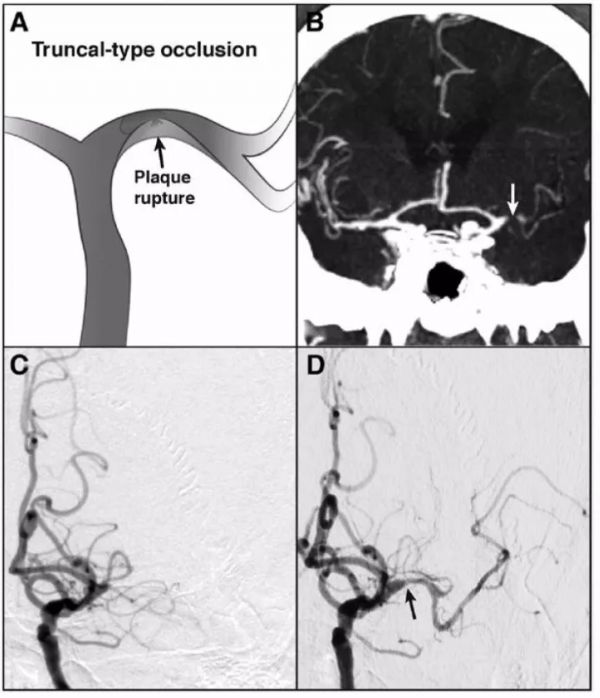
示例1:CTA干型闭塞。A图为模式图,粥样硬化斑块破裂所致MCA闭塞;B图,CTA显示MCA闭塞(箭头),MCA分叉部位未闭塞;C图,DSA显示相同部位闭塞;D图,支架取栓一次后左侧MCA再通,回收一些细小碎片;不过,DSA显示M1段主干局灶性狭窄(箭头);10分钟后再次闭塞:
示例2:CTA分支部位闭塞。A图为模式图,栓子(箭头)闭塞MCA分叉部位;B图,CTA显示左侧MCA闭塞;MCA上干和下干显影,MCA分叉部位未见显影(箭头);D图,支架取栓一次后MCA及2个分支完全再通。取栓后延迟造影未发生MCA再闭塞,左侧M1主干未见狭窄:
该研究共纳入238例患者。CTA的闭塞类型与DSA的闭塞类型匹配(P = 0.453)。房颤(OR, 2.66; 95% CI, 1.25–5.66)和CTA分支部位闭塞(OR, 8.20; CI, 3.45–19.5)是SR成功的独立预测因素。在预测SR成功方面,CTA分支部位闭塞的接受者操作特征曲线下面积(area under the receiver operating characteristic curve)(0.695)明显高于房颤(0.594,P = 0.038)和动脉高密度征(0.603,P = 0.023)。
最终作者认为,CTA分支部位闭塞与SR成功显著相关。此外,与手术前其他两项快速和容易的检查项目发现相比,CTA分支部位闭塞最能预测SR成功。
译者注:CTA干型闭塞可能与MCA动脉粥样硬化性闭塞有关。
原始出处:
Baek JH1, Kim BM2, Yoo J,et al.Predictive Value of Computed Tomography Angiography-Determined Occlusion Type in Stent Retriever Thrombectomy.Stroke. 2017 Oct;48(10):2746-2752. doi: 10.1161/STROKEAHA.117.018096. Epub 2017 Sep 1.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CTA#
40
#动脉闭塞#
47
#取栓#
40
学习了.涨知识
65