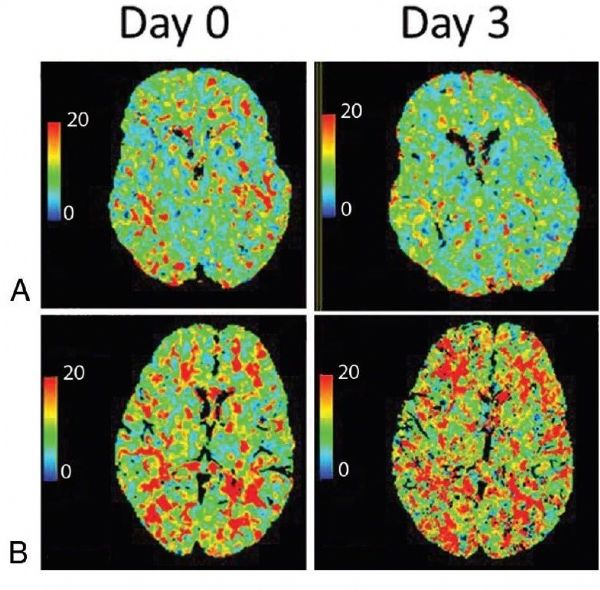
AJNR:MTT 延长预测 aSAH 后 DCI
2018-12-31 杨中华 脑血管病及重症文献导读
对于动脉瘤蛛网膜下腔出血(aSAH),识别迟发性脑缺血(DCI)高风险的患者是非常重要的,这有助于指导内科和血管内管理。管理流程大部分都是基于入院时的临床状态和 SAH 体积。 WFNS量表是常用评价临床状态的方法。高 WFNS 分级(IV-V)与较高的 DCI 和死亡风险有关,入院时较好的分级比如 WFNS 1-III 级往往风险更低。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ASA#
94
#DCI#
83
#aSAH#
63
#SAH#
88