Nature:个性化癌症疫苗在早期人体试验中表现乐观
2017-07-06 佚名 Nature自然科研
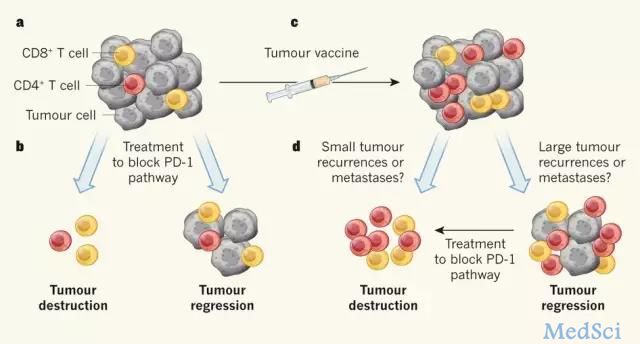
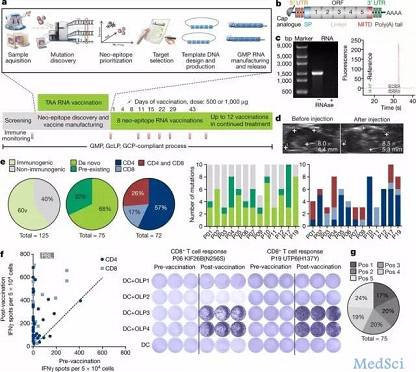
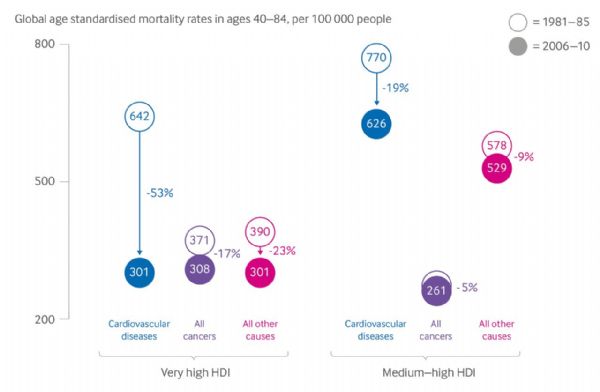
本周《自然》在线发表的两篇论文An immunogenic personal neoantigen vaccine for patients with melanoma和Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer中,展示了两种个性化的癌症疫苗的接种在小规模

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#乐观#
49
#Nat#
39
很好,不错,以后会多学习
63
学习了,谢谢分享
77
#人体试验#
51
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
74
学习了分享了
66