Eur Neurol:烟雾病中基底部侧枝形成的决定性因素:临床和遗传因素
2016-04-10 MedSci MedSci原创
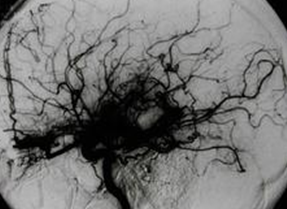
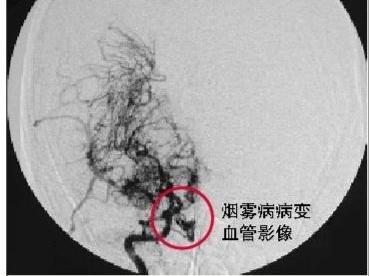
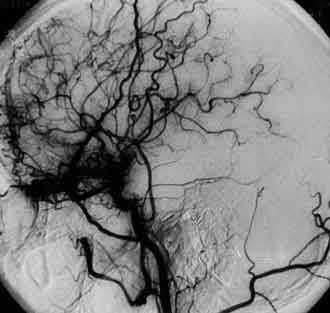
研究背景/目的:为了诊断烟雾病(MMD),需要发现颈内动脉远端狭窄和基底部侧枝(BCs)烟雾状网络。这项研究旨在评估可以决定血管造影确定为MMD的病人形成基底部侧枝程度的因素。研究方法:我们分析了连续的146例诊断为MMD的病人(年龄 26.2 ± 19.6, 1-75)。基底部侧枝形成的程度(%)基于常规的血管造影评估。基底部侧枝形成的程度相关的被分析的因素包括临床放射学和基因因素(
研究背景/目的:为了诊断烟雾病(MMD),需要发现颈内动脉远端狭窄和基底部侧枝(BCs)烟雾状网络。这项研究旨在评估可以决定血管造影确定为MMD的病人形成基底部侧枝程度的因素。
研究方法:我们分析了连续的146例诊断为MMD的病人(年龄 26.2 ± 19.6, 1-75)。基底部侧枝形成的程度(%)基于常规的血管造影评估。基底部侧枝形成的程度相关的被分析的因素包括临床放射学和基因因素(编号为4810基因编码的精氨酸被赖氨酸取代)。
研究结果:MMD病人中BCs程度各种各样,随着诊断为MMD时年龄的增加显著降低(系数为 -1.55; p < 0.001)。尽管BC发展的程度取决于MMD的阶段(Suzuki 分级),但是成人起病(>18 岁)的MMD患者与儿童起病的MMD患者相比,其程度较轻。是否存在R213基因异常,MMD类型(双侧或单侧),卒中类型(缺血性,出血性或者无症状性),颅内血管的收缩(外径),颈外动脉侧枝状态以及皮质新血管生成和BCs程度无关。
研究结论:尽管显著的BCs是诊断MMD必须的,但BCs随起病年龄递减,提示成人起病和儿童MMD血管生成能力的区别。
原始出处:
Chung JW1, Kim SJ, Bang OY, Kim KH, Ki CS, Jeon P, et al,Determinants of Basal Collaterals in Moyamoya Disease: Clinical and Genetic Factors.Eur Neurol. 2016 Apr 6;75(3-4):178-185. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#烟雾病#
0
#Neurol#
90
文章不错
159
值得学习
184
#遗传因素#
76
了解学习
190
了解学习
161