Euro Radio:微波消融在治疗原发性甲状旁腺功能亢进中的价值
2022-08-20 shaosai MedSci原创
目前的治疗指南推荐甲状旁腺切除术(PTX)作为PHPT患者的标准治疗方法。
 据统计,原发性甲状旁腺功能亢进症(pHPT)是第三大最常见的内分泌疾病,是矿物质代谢紊乱导致的相关综合症。据估计,全球每年甲状旁腺功能亢进症的发病率为每1000人中有1至4例,并有明显的性别倾向(女:男=3-4:1)。异常升高的甲状旁腺激素(PTH)和高钙血症可能引起一系列临床症状,如骨质疏松、骨折、肾结石、肾功能减退、神经认知功能受损,甚至出现高钙血症危象。近年来,随着社会经济生活条件的改善,越来越多的人开始重视常规体检,因此,无症状PHPT的检出率也随之提高。据观察,20-30%的无症状PHPT可发展为有症状的PHPT。
据统计,原发性甲状旁腺功能亢进症(pHPT)是第三大最常见的内分泌疾病,是矿物质代谢紊乱导致的相关综合症。据估计,全球每年甲状旁腺功能亢进症的发病率为每1000人中有1至4例,并有明显的性别倾向(女:男=3-4:1)。异常升高的甲状旁腺激素(PTH)和高钙血症可能引起一系列临床症状,如骨质疏松、骨折、肾结石、肾功能减退、神经认知功能受损,甚至出现高钙血症危象。近年来,随着社会经济生活条件的改善,越来越多的人开始重视常规体检,因此,无症状PHPT的检出率也随之提高。据观察,20-30%的无症状PHPT可发展为有症状的PHPT。
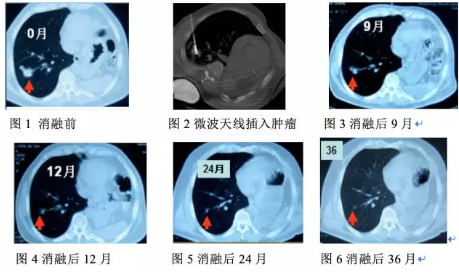
目前的治疗指南推荐甲状旁腺切除术(PTX)作为PHPT患者的标准治疗方法。近几十年来,已经有一些关于pHPT微创治疗的报道,如乙醇消融、激光消融、射频消融和高强度聚焦超声。作为热消融技术中最新的、令人振奋的进展之一,微波消融(MWA)已被常规应用于pHPT的治疗。大多数研究表明,MWA可以有效地灭活pHPT结节,使血清PTH、钙和磷恢复正常。然而,受限于样本量小和随访时间短,治疗效果的确切证据并不详实。
近日,发表在European Radiology杂志的一项研究使用更大的样本量、更长的随访时间进一步对MWA和PTX进行了比较研究,分析了复发和顽固性PHPT的可能风险因素以获得关于MWA治疗PHPT的更明确的结果,并获得了更多预防手术失败的技术细节。
本项回顾性研究在2015年1月至2020年10月期间招募了212名由MWA(MWA组)或PTX(PTX组)治疗的pHPT患者。基线数据通过倾向性评分匹配得到平衡。通过Kaplan-Meier方法评估临床治愈情况,并在MWA组和PTX组之间进行比较。采用Cox比例危害回归模型筛选出与持续或复发PHPT有关的风险因素。
经过倾向性评分匹配,共有174名患者被纳入本研究,每组有87名患者。在随访期间(中位数,28.5个月),两组在临床治愈率(危险比,1.71;95%置信区间:0.81-3.62;P = .155)、PHPT持续率(13.8% vs. 10.3%,P = .643)、PHPT复发率(6.9% vs. 3.4%,P = .496)或主要并发症(6.9% vs. 3.4%,P = .496)方面没有差异。MWA的手术时间较短(30分钟对60分钟)、切口长度较小(0.1厘米对7厘米)、费用略高(25745元人民币对24111元人民币)(所有P < .001)。术前完整的甲状旁腺激素水平高(p = .01)和多个pHPT结节(p < .001)是两组中复发和持续pHPT的独立风险因素。
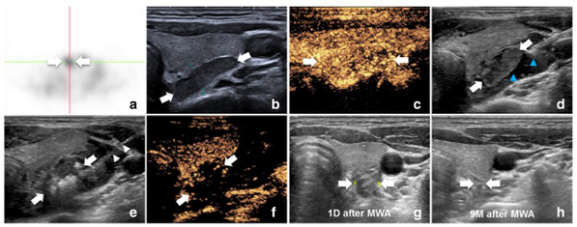
图 图片显示pHPT结节的MWA手术。a MIBI上pHPT结节有放射性浓聚(白色箭头)。b 超声显示甲状腺右侧低回声pHPT结节(白色箭头)。e 消融过程:在pHPT结节内部出现(白色箭头)周围的高回声区(白色箭头)。f CEUS显示覆盖pHPT结节的非增强区(白色箭头)。g MWA后一天消融区(2.0cm × 0.9cm)。h MWA后九个月,消融区被吸收
本研究表明,MWA和PTX在治疗pHPT的疗效和并发症方面是相当的。MWA是一项微创手术,且手术时间较短。本研究同时发现,多发性结节和高水平的血清iPTH是复发和持续的pHPT的风险因素。
原文出处:
Ying Wei,Zhen-Long Zhao,Xiao-Jing Cao,et al.Microwave ablation versus parathyroidectomy for the treatment of primary hyperparathyroidism: a cohort study.DOI:10.1007/s00330-022-08759-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#原发性#
49
#甲状旁腺功能亢进#
53
#消融#
59
#甲状旁腺#
47
#原发性甲状旁腺功能亢进#
43