可逆性胼胝体压部病变综合征影像1例
2019-08-06 不详 影像园
患者3天无明显诱因出现发烧,自量体温37.8度,无明显呕吐,进半天频繁抽搐不缓解。入院查体:神经系统体征未见明显阳性征象。
【所属科室】
神经内科
【基本资料】
患者,女,8岁
【主诉】
感冒3天,近半日抽搐6次
【现病史】
患者3天无明显诱因出现发烧,自量体温37.8度,无明显呕吐,进半天频繁抽搐不缓解。入院查体:神经系统体征未见明显阳性征象。
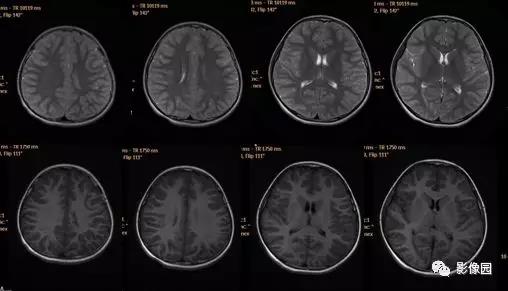
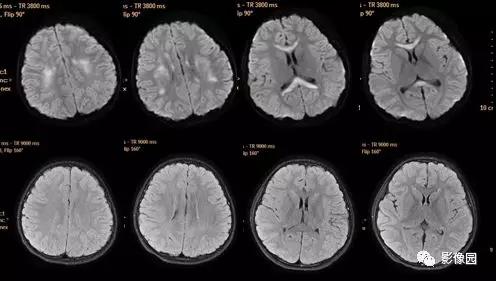
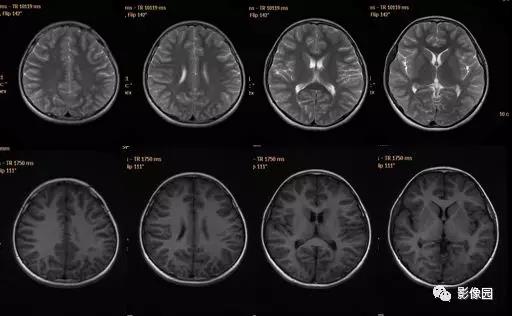
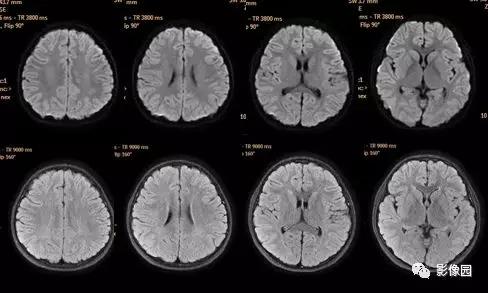
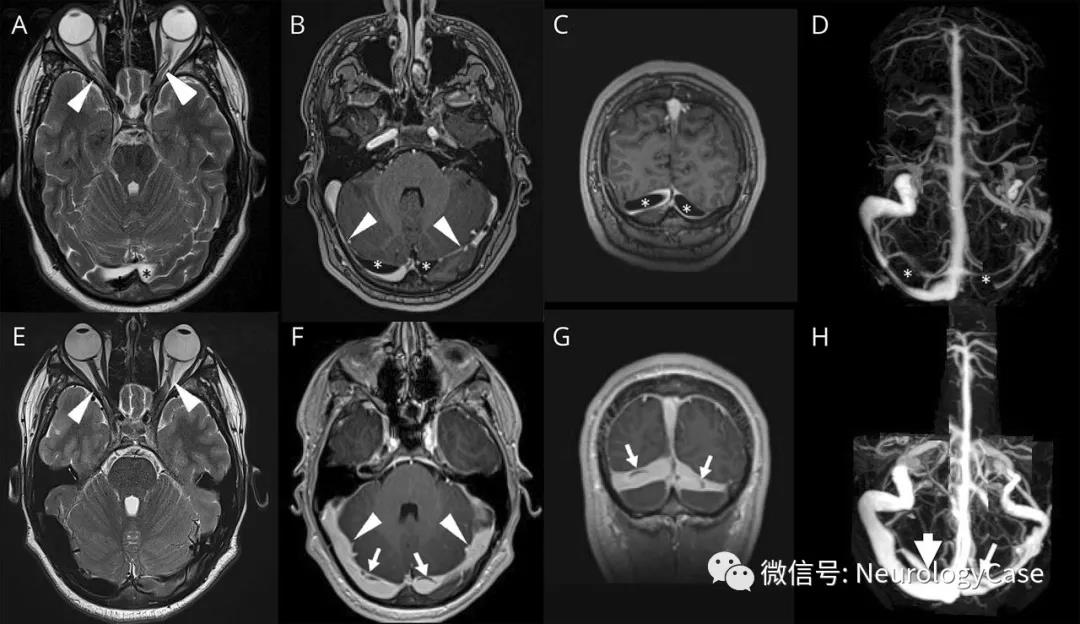
【影像图片】


【影像表现】
胼胝体及双侧半卵圆中心多发斑片状、条片状稍长T1稍长T2信号影 ,信号较均匀,T2flair呈稍高信号 ,DWI呈高信号 ,ADC图呈明显低信号 。治疗后复查异常信号消失。
【结果】
【病例小结】
可逆性胼胝体压部病变综合征是一种急性单病程的非特异性脑炎/脑病综合征,是一种以胼胝体压部( SCC) 可逆性病变为主要特点的临床影像综合征。国外报道较多,尤其以日本多见 目前国内对该病报道较少,以成人为主成人及儿童均可发病,男女发病比例无明显差异。癫痫及其相关因素--癫痫发作、使用抗癫痫药物、抗癫痫药物撤药(最多见)根据受累部位可分为2型:1型--仅有胼胝体压部受累,此型多见;2型-除胼胝体压部受累外,其他部位白质也可受累,此型少见;临床表现无特异性,主要表现为轻微脑炎或脑病; 可仅表现发热、头痛、呕吐等非典型症状; 也可出现脑实质损害,表现为意识障碍、抽搐、谵妄、同向偏盲、共济失调及眩晕; 临床过程良性,一般1周内临床症状消失,1个月内痊愈。 日本学者Tada 2004年提出的诊断标准: 相对轻微的中枢神经系统症状,如谵妄、轻度意识障碍;颅脑MRI表现为胼胝体压部出现DWI高信号或ADC低信号;症状迅速缓解,1个月内完全恢复。影像学检查发现胼胝体压部可逆性病灶是本病的特征性改变,DWI或ADC能提供较早期的胼胝体压部病变影像特征性表现:DWI或ADC出现可逆性胼胝体压部的弥散受限,治疗后头颅MRI 异常信号均吸收消失。需要与以下疾病鉴别:胼胝体梗死:多见于成人患者多有脑血管病危险因素,胼胝体压部为大脑后动脉和脉络膜后动脉供血,因此,胼胝体压部梗死多伴枕叶及颞叶梗死,单独受累者少见。原发性胼胝体变性,一种罕见脱髓鞘性疾病,多见于成人酗酒者发病机制尚不明确,影像学累及部位不仅局限于压部,临床表现可有震颤、精神异常、意识障碍等,表现为慢性病程,询问饮酒史对其诊断较为重要。可逆性后头部脑病综合征,多见于恶性高血压及肿瘤患者抗肿瘤药物应用后,临床表现剧烈头痛、意识障碍、癫痫及视力受损,病因多样,顶枕叶受累脑白质为血管源性水肿,病程具自限性,预后一般较好。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胼胝体#
133
#胼胝体压部#
149
#病变综合征#
120
#综合征#
122
#可逆性#
126