NEJM:严重左侧膈疝胎儿手术的随机试验
2021-06-09 MedSci原创 MedSci原创
先天性膈疝的患病率约为1/4000,即每4000名新生儿中有1人将会患此病。在膈肌发育过程中,如胚胎时的裂隙未能完全闭合,而在横膈上遗留成为裂孔,即可形成疝。在先天性膈疝的
先天性膈疝的患病率约为1/4000,即每4000名新生儿中有1人将会患此病。在膈肌发育过程中,如胚胎时的裂隙未能完全闭合,而在横膈上遗留成为裂孔,即可形成疝。在先天性膈疝的病例中,有85%左右的患者缺损部位于左侧。在先天性膈疝中,腹部内脏的胸内疝会损害正常气道和肺血管的发育。 因此,这种情况与新生儿因呼吸衰竭和肺动脉高压而死亡高度相关。存活下来的婴儿可能会出现严重的健康并发症,包括胃肠道和呼吸系统问题、骨科畸形和神经发育迟缓。对于先天性膈疝儿童,需要终身多学科随访以早期诊断和处理并发症。在美国,先天性膈疝患者的产后护理费用每年超过 2.5 亿美元,使其成为最昂贵的非心源性天生缺陷。
对于患有先天性膈疝的胎儿,出生后存活结果的产前评估主要是通过其他主要缺陷及是否存在染色体异常、肺大小的测量以及通过超声或磁共振成像检查或确定是否存在胸腔内肝脏来确定的。肺大小通常根据对侧肺面积(在二维超声扫描显示心脏的标准四腔视图中测量)与头围的比值进行评估。由于这些测量值总是随胎龄而变化, 肺大小更好地表示为观察/预期的肺头比的商(即观察到的肺面积与头围的比值 [通过超声测量] 除以相同胎龄的健康胎儿肺头比的比值)。观察/预期的肺头比的商数小于 25.0% 的胎儿意味着严重肺发育不良,其存活机会小于 25%。观察/预期的肺头比的商也可以预测早期新生儿并发症,例如延长使用通气和补充氧气的需要,以及完全肠内喂养的时间。
正如先天性高位气道阻塞以及实验性胎儿气管结扎后所观察到的那样,已经发现气管阻塞会刺激胎儿肺生长。实验还表明,产前逆转阻塞和使用糖皮质激素能够促进肺成熟。临床上的气管阻塞,最初是通过在母亲全身麻醉时使用外部夹子实现的。 研究人员因此开发了一种胎儿镜管腔内气管闭塞 (FETO) 技术,包括在管腔内插入充气球囊,几周后移除球囊; 此项技术可以在母体处于局部麻醉状态下进行。
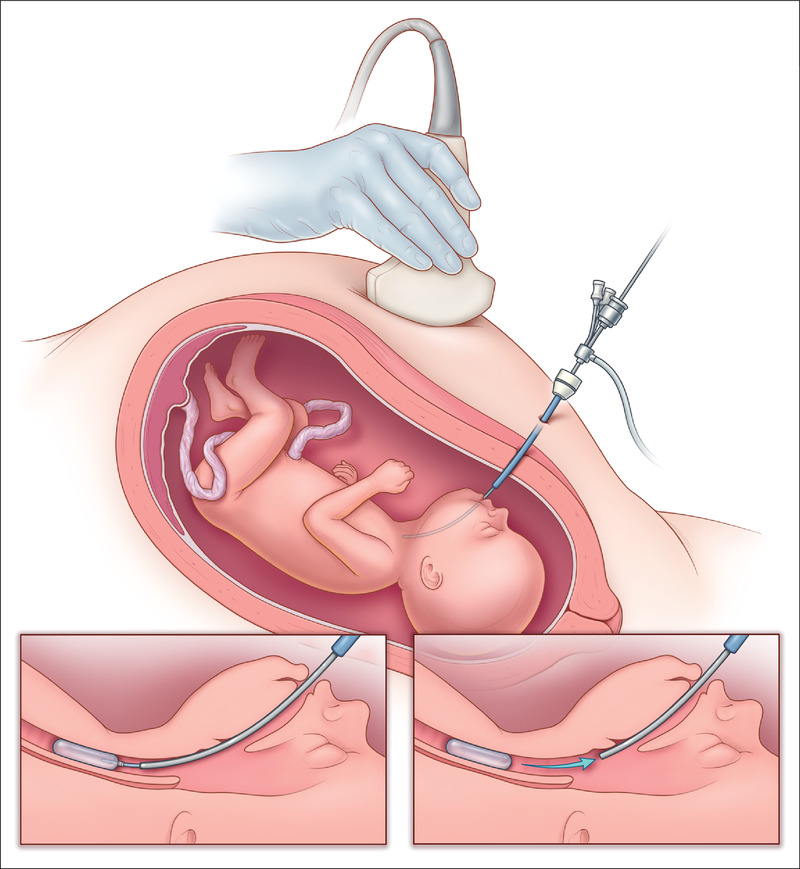
在一项涉及 210 名因孤立性先天性膈疝而严重发育不全的胎儿的研究中,使用 FETO(在大约 28 周时插入气囊并在 34 周时取出)似乎对母亲具有可接受的安全性。 与历史对照相比,这些胎儿的新生儿存活率高于历史对照(49% vs. 24%),早期新生儿呼吸道并发症的发生率较低,但早产风险较高。 研究人员设计了气管闭塞加速肺生长 (TOTAL) 试验(www.totaltrial.eu.opens in new tab)来检验以下假设:在由于左侧孤立的先天性膈疝导致严重肺发育不良的胎儿中,使用 FETO可能会增加产后存活率。

在这项在具有 FETO 和其他类型产前手术经验的中心进行的开放标签试验中,研究人员以 1:1 的比例将左侧严重孤立性先天性膈疝的27-29孕周单胎孕妇随机分配到 FETO 组或期待护理组。 两种治疗后均进行标准化的产后护理。 主要结果是婴儿从新生儿重症监护病房出院的存活率。研究人员使用了一组序列设计,其中包含五个预先指定的中期优势分析,最大样本量为 116 名女性。
在第三次中期分析后,该试验因疗效而提前停止。 在一项纳入 80 名女性的意向治疗分析中,FETO 组中有 40% 的婴儿(40 名中的 16 名)存活出院,而期待护理组中这一数据为 15%(40 名中的 6 名)(相对风险,2.67 ;95% 置信区间 [Cl],1.22 至 6.11;双侧 P=0.009)。6 个月的存活率与出院的存活率相同(相对风险,2.67;95% Cl,1.22 至 6.11)。FETO 组妇女的早产、临产前胎膜破裂的发生率(47% 对 11%;相对风险,4.51;95% Cl,1.83 至 11.9)和早产发生率(75% 对 29%;相对风险,2.59;95% Cl,1.59 至 4.52)均高于期待护理组。1例新生儿因胎儿镜下球囊摘除引起胎盘撕裂而急诊分娩后死亡,1例新生儿因球囊摘除失败而死亡。在包括 11 名试验停止后可获得数据的额外参与者的分析中,FETO 组婴儿的出院存活率为 36%,期待护理组婴儿的出院存活率为 14%(相对风险,2.65;95% Cl,1.21 到 6.09)。
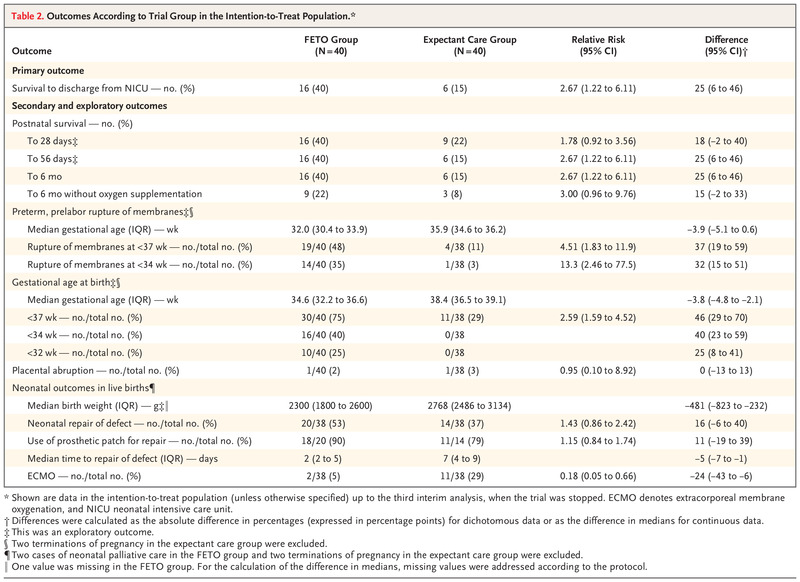
实验结果表明,在左侧有孤立的严重先天性膈疝的胎儿中,在妊娠 27 至 29 周进行的 FETO 在出院存活率方面比期待护理有显着益处,并且这种益处持续到 6 个月大。但FETO 增加了胎膜早破和早产的风险。
原文链接:https://www.nejm.org/doi/full/10.1056/NEJMoa2027030?query=featured_home
Randomized Trial of Fetal Surgery for Severe Left Diaphragmatic Hernia List of authors.
Jan A. Deprest, M.D., Ph.D., Kypros H. Nicolaides, M.D.June 8, 2021 DOI: 10.1056/NEJMoa2027030
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#随机试验#
105
#疝#
78
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
74
高质量研究,读起来真爽,谢谢梅斯
86
真的学习
95
学习
95