AJRCCM:小儿心脏重症监护病房的肺动脉高压导致的死亡率
2021-10-15 刘少飞 MedSci原创
患有肺动脉高压 (PH) 的儿童代表了越来越多的住院患者,其发病率和死亡率都很高。门诊治疗的进步改善了结果,但也提高了对住院后生存的期望。儿科 PH 的病因是异质的,但最终常见的病理生理学是右心室衰竭

患有肺动脉高压 (PH) 的儿童代表了越来越多的住院患者,其发病率和死亡率都很高。门诊治疗的进步改善了结果,但也提高了对住院后生存的期望。儿科 PH 的病因是异质的,但最终常见的病理生理学是右心室衰竭,这些儿童在介入手术后、麻醉后和急性内科疾病后心脏骤停的风险特别高。因此,住院管理经常需要入住 ICU。
专门的儿科心脏重症监护病房 (PCICU) 通常会照顾这些儿童,但关于这种情况下的结果和医院课程的数据仍然很少。来自普通儿科 ICU (PICU) 人群的先前文献表明,PH 儿童在死亡率、住院时间更长和侵入性干预(包括心肺复苏 (CPR)、体外膜肺氧合 (ECMO))方面的风险显着高于非 PH 儿童和机械通风。入住 PCIICU 的儿童可能代表不同的人群,包括更多患有潜在结构性心脏病和严重心功能不全的儿童。认识到与 PCICU 环境中死亡率增加相关的因素将为护理这一高危患者群体的从业者提供重要的新见解。
在此背景下,我们对小儿心脏重症监护联盟 (PC4) 注册进行了回顾性分析,该注册维护来自北美 PCICU 的多中心数据库。我们旨在描述因医疗指征而入住 PCIICU 的 PH 儿童的特征和结局,确定与 PCICU 死亡率增加相关的因素,并评估早期接受重症监护治疗与死亡率的相关性。这些研究的一些结果之前已经以摘要的形式报道过。
研究目的:确定与 PH 心脏重症监护入院死亡率相关的因素。
研究方法:该研究评估了 5 年来儿科心脏重症监护联盟机构的 PH 入院率。 PH 在临床登记中通过诊断和/或接受重症监护级别的肺血管扩张剂治疗来标准定义。
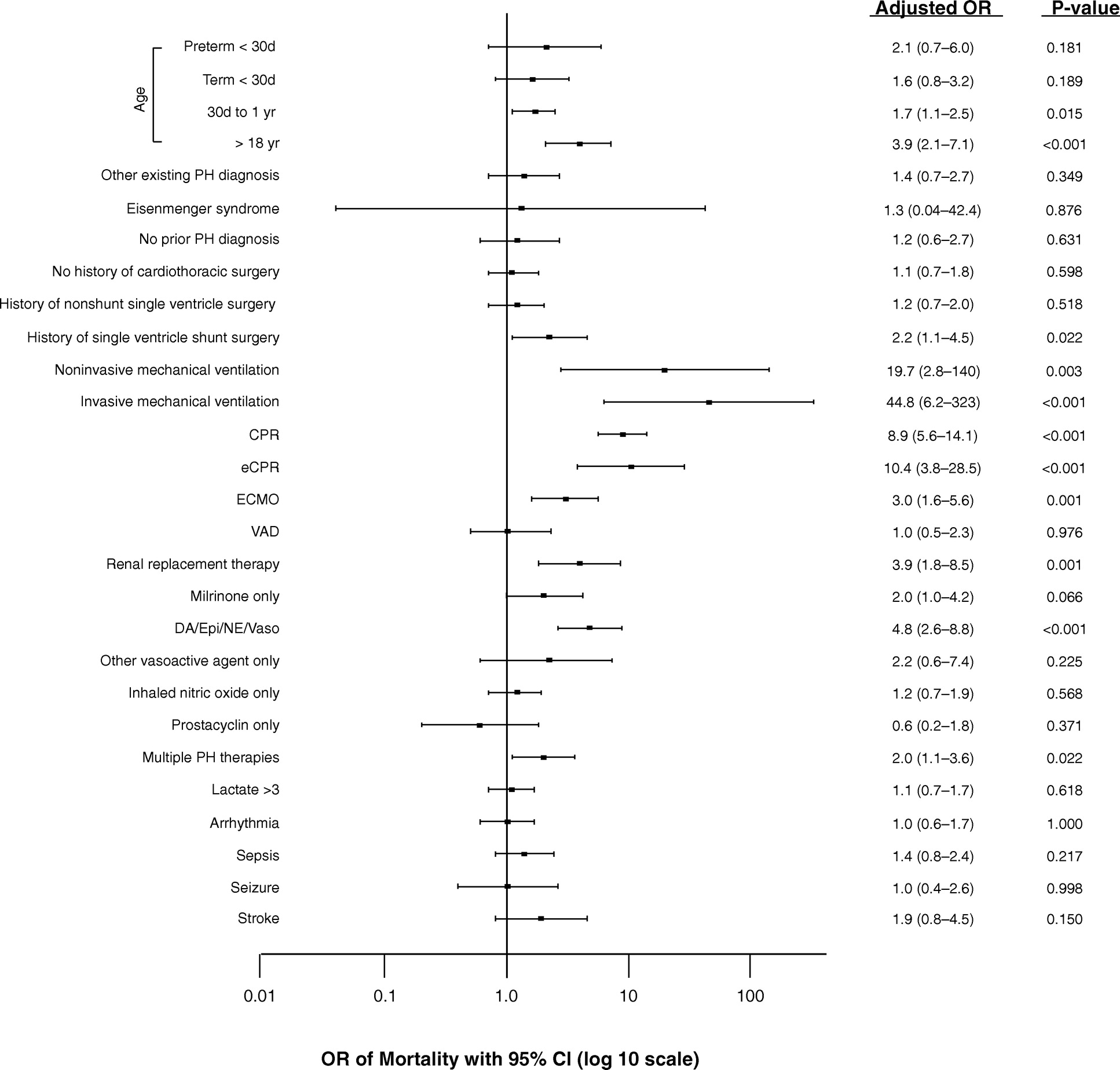
研究主要结果:该研究分析了 2,602 名入院者;死亡率为 10%,而所有其他医疗入院的死亡率为 3.9%。与死亡率最相关的协变量包括有创通气(调整比值比,44.8;95% 置信区间,6.2-323)、无创通气(19.7;2.8-140)、心肺复苏(8.9;5.6-14.1)和血管活性输注( 4.8;2.6–8.8)。在入院第 1 天和第 2 天接受有创通气和血管活性药物输注的患者观察到的死亡率分别为 29.2% 和 28.6%,而未接受这两种治疗的患者死亡率均<5%。血管活性药物输注成为主要的早期死亡风险因素,入院第 2 天出现时,死亡绝对风险平均增加 6.4%。
研究结论:入住儿科心脏重症监护病房的 PH 患者死亡率很高。 在第 1 天或第 2 天接受有创通气和血管活性药物输注的患者观察到的死亡率是未接受有创通气和血管活性药物的患者的 5 倍以上。 这些数据突出了在这种情况下 PH 患者的疾病严重程度,并有助于与家人就预后进行对话。
文章出处:
Morell E, Gaies M, Fineman JR, Charpie J, Rao R, Sasaki J, Zhang W, Reichle G, Banerjee M, Tabbutt S. Mortality from Pulmonary Hypertension in the Pediatric Cardiac ICU. Am J Respir Crit Care Med. 2021 Aug 15;204(4):454-461. doi: 10.1164/rccm.202011-4183OC. PMID: 33798036.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉高压#
49
#RCC#
61
#重症监护病房#
66
#监护#
69
#学习#赞
67