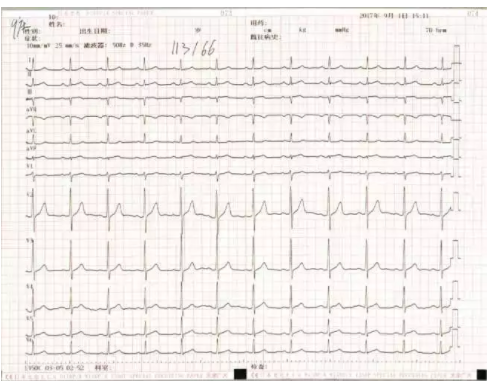
CCIF2018丨特约病例:STEMI精准再通新策略——冠状动脉内溶栓治疗急性心肌梗死1例
2018-04-21 国际循环编辑部 国际循环
2018年4月20~22日,第二十一届全国介入心脏病学论坛(CCIF 2018)于宁夏银川召开。本届会议日程丰富多彩,设置多场病例讨论,专家们通过典型、疑难病例分享诊疗经验,探讨最佳治疗方案。河北医科大学第二医院汪雁博在大会报告了1例关于STEMI精准再通新策略的精彩病例。





本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CCIF#
75
#动脉内溶栓#
63
#精准#
62
#溶栓治疗#
66
#新策略#
85
#STEM#
85
学习一下谢谢
92
好文献.学习了
87
不错.学习了.做笔记了.谢谢分享!
86
好文.值得点赞!认真学习了.把经验应用于实践.为患者解除病痛.
99