大脑淀粉样血管病(CAA)的特点是淀粉样β(Aβ)在小动脉和动脉血管的内膜和毛细血管的基底膜上沉积,可能是由于Aβ的清除功能受损。

因此,血管壁变弱,导致血脑屏障(BBB)的完整性受损,血液以大叶脑微出血(CMBs)和脑内出血(ICHs)的形式外渗到实质。目前,生活中CAA的诊断是基于修改后的波士顿标准,用磁共振成像(MRI)标记CAA的出血性表现。然而,这些都是CAA相对晚期的间接标志,它们并不能提供该疾病的确切证据。
脑脊液(CSF)标志物可能提供了一个在早期阶段识别CAA的机会,并可能使这种生物标志物用于监测脑血管Aβ病理学的进展。CSF血小板源性生长因子受体-β(PDGFRβ)是CAA的一个潜在生物标志物。PDGFRβ被认为是周细胞的生物标志物,而脑周细胞在BBB的饱和度和维持方面有关键作用。
此外,在轻度认知障碍(MCI)患者中,使用动态对比增强MRI(DCE-MRI),CSF中PDGFRβ水平的增加与BBB通透性的增加有关。
另外,CSF PDGFRβ的浓度在MCI患者(定义为临床痴呆评分[CDR]为0.5分)中有所增加,在痴呆患者(CDR为1.0分)中增加到更高水平。
此外,在具有AD+生物标志物(定义为CSF Aβ42、磷酸化tau[p-tau]和总tau[t-tau]水平异常;认知状态未知)的参与者中,与没有这种生物标志物的对照组相比,CSFPDGFRβ水平增加。
藉此, 荷兰🇳🇱拉德堡德大学医学中心(Radboudumc)的 Anna de Kort等人,探究了:
(1)CAA患者的CSF PDGFRβ水平与对照组相比是否升高;
(2)验证以前描述的结果:只有在无记忆性MCI(aMCI)患者(CDR 0.5)、轻度痴呆的AD患者(CDR 1. 0)和中度痴呆(CDR 2.0)的AD患者
(3)与没有这种特征的对照组相比,验证具有AD+生物标志物特征的aMCI/AD患者的CSF PDGFRβ水平
他们通过酶联免疫吸附法对CAA患者、aMCI/AD患者以及匹配的对照组的CSF PDGFRβ水平进行了定量分析。
在aMCI/AD中,他们通过临床表型和使用由CSF淀粉样蛋白(A)、tau(T)和神经变性(N)生物标志物定义的AT(N)生物标志物分类系统评估CSF PDGFRβ。
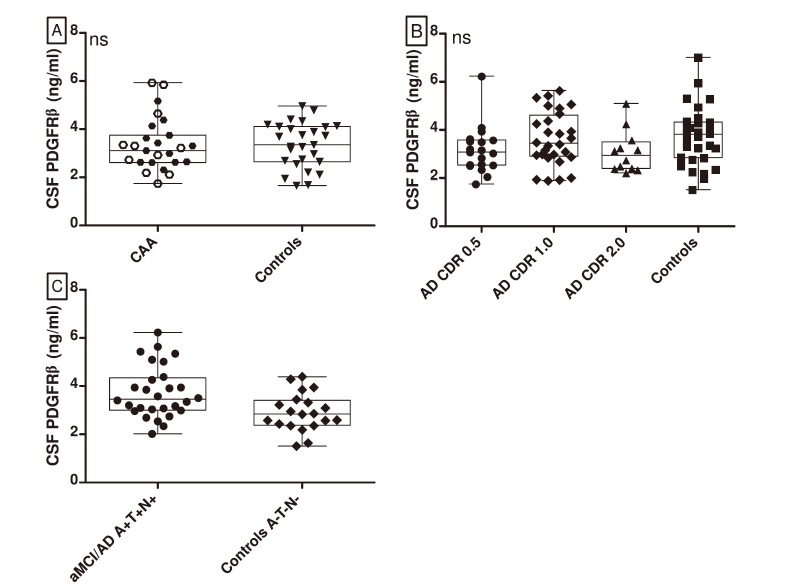
他们发现: PDGFRβ水平在CAA患者和对照组中相似(P = .78),在aMCI/AD临床表型和对照组中相似(P = .91)。
与(A-T-[N-])对照组相比,具有AD+生物标志物特征的aMCI/AD患者的PDGFRβ水平有所增加(P = .006)。
该研究结果表明,PDGFRβ水平与AD+生物标志物特征有关,但不是CAA或aMCI/AD临床综合征的合适生物标志物。
原文出处:
De Kort AM, Kuiperij HB, Kersten I, et al. Normal cerebrospinal fluid concentrations of PDGFRβ in patients with cerebral amyloid angiopathy and Alzheimer’s disease. Alzheimer’s & Dementia. Published online December 7, 2021:alz.12506. doi:10.1002/alz.12506
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#dementia#
84
#标志物#
75
#阿尔兹海默#
94
#GFR#
74
#生物标志#
84
#生物标志#
73