视网膜的变化可能与健康受试者患阿尔茨海默病风险的大脑部分有关
2022-08-17 brainnew神内神外 阿尔茨海默病
除了视网膜的结构,UCM 小组还在收集患者视力的数据,以发现视觉网络在这些仍无症状的疾病阶段是如何运作的。

在认知健康但遗传风险较高的阿尔茨海默病受试者中,视网膜与因疾病而发生变化的各种大脑结构如(内嗅皮层、舌回和海马体)之间的相关性已得到证实。

《神经科学新闻》7月26日消息
这是马德里康普顿斯大学(Complutense University of Madrid,UCM) Ramón Castroviejo 眼科研究所(IIORC)领导的研究的主要结论。
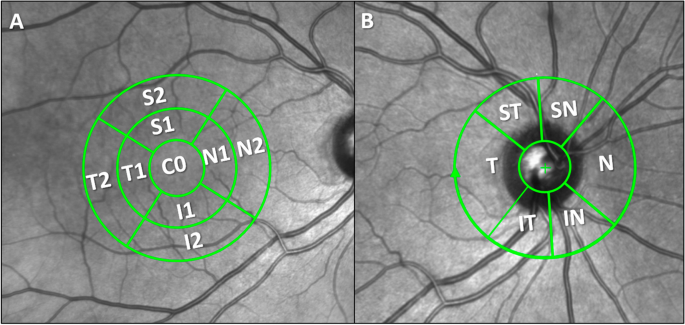
这项发表在《阿尔茨海默病研究与治疗》(Alzheimer's Research & Therapy)杂志上的研究的新奇之处在于,它第一次检查了视网膜区域和阿尔茨海默病中受影响最严重的大脑结构之间的相关性。阿尔茨海默病在首次症状出现之前可能会经过长达 20 年的时间。

研究于2022年6月4日发表在《Alzheimer's Research & Therapy》(最新影响因子:8.823)杂志上
该研究的主要作者、IIORC 研究员 Inés López-Cuenca 指出:“这意味着视网膜是一种容易接近的组织,它可能提供有关大脑状态和其中发生的变化的信息。”
San Carlos 临床医院和马德里理工大学(Technical University of Madrid,UPM)参与了 UCM 的研究,作为 COGDEM 研究的一部分。
下一步:研究视觉
为了进行这项研究,研究人员选取了一组患者,他们的父亲或母亲都患有阿尔茨海默病,而且他们的 ApoEɛ4 基因有突变,这种突变使他们容易患上阿尔茨海默病。
IIORC 对他们进行眼科检查,包括光学相干断层扫描(OCT)。然后,这些测试与马德里 San Carlo 大学临床医院神经科进行的磁共振成像(MRI)进行比较,测量了两个大脑半球 20 多个不同的大脑结构。

López-Cuenca 说:“我们已经看到,这些参与者已经显示出用 OCT 测量的视网膜的某些区域发生了变化,而大脑磁共振成像仍然正常。”
除了视网膜的结构,UCM 小组还在收集患者视力的数据,以发现视觉网络在这些仍无症状的疾病阶段是如何运作的。
参考文献
Source:Complutense University of Madrid
Changes in the retina can be linked to parts of the brain of healthy subjects at risk of Alzheimer’s
Reference:
López-Cuenca, I., Marcos-Dolado, A., Yus-Fuertes, M. et al. The relationship between retinal layers and brain areas in asymptomatic first-degree relatives of sporadic forms of Alzheimer’s disease: an exploratory analysis. Alz Res Therapy 14, 79 (2022). https://doi.org/10.1186/s13195-022-01008-5
- END -
取消 允许
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阿尔茨海#
67
#阿尔茨#
69
#视网膜#
71
#受试者#
77
#阿尔茨海默#
62