NEJM:Sotorasib治疗KRASp.G12C突变晚期非小细胞肺癌II期临床数据喜人
2021-06-07 MedSci原创 MedSci原创
Sotorasib在先前接受过铂化疗或免疫治疗的KRASp.G12C突变非小细胞肺癌患者中表现出良好的治疗效果且安全性良好

近年来,得益于靶向药物及免疫疗法,非小细胞肺癌(NSCLC)的治疗取得了显著进展,患者死亡率大幅下降,但晚期NSCLC患者的预后仍不令人满意,中位无进展生存期仅为2至4个月。对于接受过铂基础化疗和免疫检查点抑制剂后病情仍进展的患者,目前的一线治疗手段仍是紫杉醇类药物。Sotorasib是首个进入临床试验的KRAS抑制剂,在I期临床研究中,Sotorasib在KRASp.G12C突变的晚期实体瘤患者中显示出抗癌活性,在非小细胞肺癌(NSCLC)患者亚组中观察令人欣喜的抗癌活性。近日研究人员公布了Sotorasib治疗KRAS p.G12C突变晚期NSCLC患者的II期临床研究数据。
在本次单中心II期试验中,研究人员考察了Sotorasib对先前接受标准治疗的KRAS p.G12C突变晚期NSCLC患者的疗效,患者每日接受一次960mg的药物治疗。研究的主要终点是客观反应(完全或部分反应),关键次要终点包括反应持续时间、疾病控制(定义为完全反应、部分反应或稳定疾病)、无进展生存期、总生存期和安全性。
126名患者中,大多数(81.0%)曾接受过铂类化疗和或PD-1/PD-L1治疗,124名患者进行了疗效评估。46例患者对治疗有应答(37.1%),其中完全缓解4例(3.2%),部分缓解42例(33.9%),中位缓解时间为11.1个月,100例患者的病情得到控制 (80.6%),中位无进展生存期为6.8个月,中位总生存期为12.5个月。126例患者中88例(69.8%)发生治疗相关不良事件,其中3级事件25例(19.8%),4级事件1例(0.8%)。
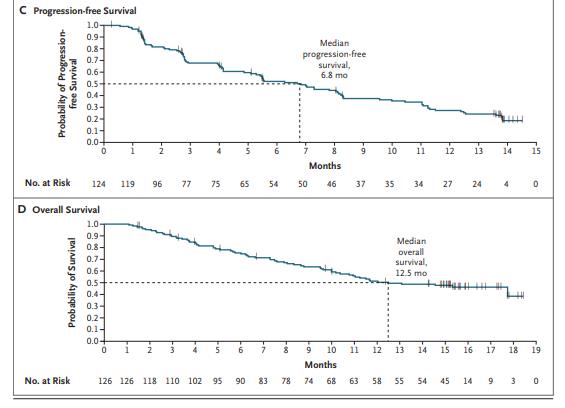
Sotorasib治疗后无进展生存期,总生存期数据
研究认为,Sotorasib在先前接受过铂化疗或免疫治疗的KRASp.G12C突变非小细胞肺癌患者中表现出良好的治疗效果且安全性良好。
原始出处:
Ferdinandos Skoulidis et al. Sotorasib for Lung Cancers with KRAS p.G12C Mutation. N Engl J Med,June 4,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#非小细胞#
94
#临床数据#
113
#RASI#
83
已读,真是受益匪浅呀。
118
#I期临床#
89
#KRAS#
91
#II期临床#
104
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
80
学习了
95