本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

2019-08-29 小通 生物通
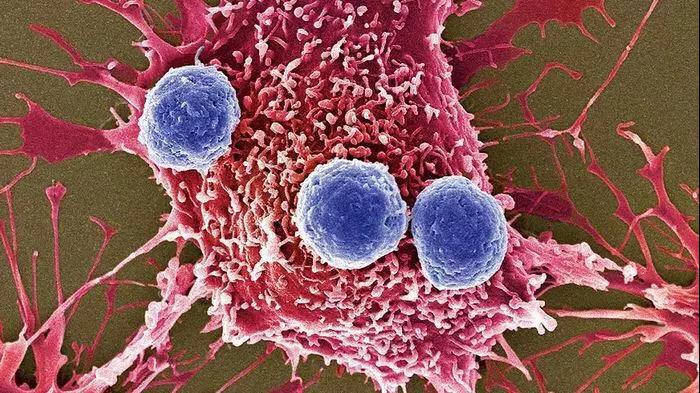
在乳腺癌对免疫疗法的抗性中发现了多种免疫细胞的不同作用

华威大学沃里克医学院Greaves实验室与爱丁堡大学的合作者一起,发现巨噬细胞在刺激神经细胞生长和活动的过程中发挥作用,导致骨盆疼痛。
韩国釜山Inje大学釜山白医院眼科疾病T2B基础设施中心的Park EY等人近日在Immunopharmacol Immunotoxicol杂志上发表了一篇文章,他们研究了硫糖肽对脂多糖(LPS)诱导的巨噬细胞系RAW 264.7炎症反应的影响,并阐明了其分子机制。
红细胞岛(EBI),由中心的巨噬细胞和周围的红细胞组成,是发现的第一个造血生态位。但迄今为止,EBI巨噬细胞的作用尚不明确。鉴于促红细胞生成素(Epo)对红细胞生成至关重要,而Epor在多种非红细胞中均有表达,研究人员推测EBI巨噬细胞可表达Epor,Epo就可以同时作用于红细胞和EBI巨噬细胞,以确保高效的红细胞生成。
心肌梗塞(MI)后的心力衰竭仍然是全世界死亡的主要原因之一,且治疗方法较棘手。本研究的目的旨在评估心梗后膜联蛋白A1(AnxA1)诱导的心脏修复的潜在治疗价值。本研究通过左冠脉结扎对AnxA1敲除小鼠(AnxA1-/-)和野生型小鼠诱导心梗。分析结果显示,AnxA1-/-小鼠表现出心脏功能减退和缺血区促炎巨噬细胞的扩张。来自Anxa1-/-小鼠的心脏巨噬细胞表现出明显降低释放血管生成前介质血管内皮
膜结合纤溶酶被免疫细胞用来降解细胞外基质,促进细胞迁移。免疫细胞,包括单核细胞和巨噬细胞,表达纤溶酶原受体Plg-RKT。根据细胞表面标志物和病理生理功能可区分单核细胞和巨噬细胞这两个不同的亚集Barbara Thaler等人对单核细胞和巨噬细胞亚群Plg-RKT的表达,以及潜在的差异表达是否可能对细胞迁移产生功能影响进行研究。与其他相关亚群相比,促炎CD14+CD16+人单核细胞和Ly6Chig
肌动蛋白结合蛋白FLNA (细丝蛋白 A)调控细胞运动过程中重要的信号转导,但巨噬细胞特异性FLNA在动脉粥样硬化形成过程中的作用尚不明确。研究人员通过免疫荧光分析了FLNA在人颈动脉粥样硬化斑块中的表达,建立巨噬细胞特异性敲除Flna的小鼠模型(Flnao/fl)。研究人员通过将雄性(Flnao/fl/LC)小鼠骨髓移植到致动脉粥样硬化性低密度脂蛋白受体缺陷(Ldlr-/-)小鼠体内,和AdPC


梅斯医学MedSci APP
医路相伴,成就大医
#Bio#
0
#Nat#
57
#CEL#
52
#Biol#
55
#Cell#
55