梅斯医学受邀参与第二届积水潭血管论坛
2016-04-26 MedSci MedSci原创
2016年4月22日,由北京积水潭医院血管外科主办的第二届积水潭血管论坛在北京·国家会议中心召开。来自相关领域的中外学者、专家齐聚一堂,共襄此次盛会。 本届积水潭血管论坛由北京积水潭医院血管外科刘建龙主任担任主席,同时本届论坛还邀请到了美国匹兹堡大学医疗中心的Rabih Chaer教授、纽约大学医学中心的Paul Gagne教授、台北慈济医院的吴典育教授以及领衔我国血管外
2016年4月22日,由北京积水潭医院血管外科主办的第二届积水潭血管论坛在北京·国家会议中心召开。来自相关领域的中外学者、专家齐聚一堂,共襄此次盛会。
 本届积水潭血管论坛由北京积水潭医院血管外科刘建龙主任担任主席,同时本届论坛还邀请到了美国匹兹堡大学医疗中心的Rabih Chaer教授、纽约大学医学中心的Paul Gagne教授、台北慈济医院的吴典育教授以及领衔我国血管外科众多学会的知名专家教授汇聚一堂。梅斯医学(MedSci)也受邀参与了本届论坛。
本届积水潭血管论坛由北京积水潭医院血管外科刘建龙主任担任主席,同时本届论坛还邀请到了美国匹兹堡大学医疗中心的Rabih Chaer教授、纽约大学医学中心的Paul Gagne教授、台北慈济医院的吴典育教授以及领衔我国血管外科众多学会的知名专家教授汇聚一堂。梅斯医学(MedSci)也受邀参与了本届论坛。


 纽约大学医学中心Paul Gagne教授与梅斯医学市场经理Ada合影
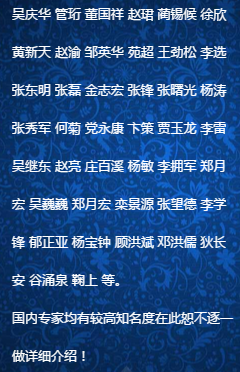
本届论坛的主题是“中美两国、海峡两岸VTE高端交流”。在论坛现场,学术氛围浓郁,来自中美两国、海峡两岸的血管外科专家们针对VTE的诊疗现状及焦点问题展开了一系列高规格、近距离交流,共同探讨了未来VTE诊治及研究方向。
纽约大学医学中心Paul Gagne教授与梅斯医学市场经理Ada合影
本届论坛的主题是“中美两国、海峡两岸VTE高端交流”。在论坛现场,学术氛围浓郁,来自中美两国、海峡两岸的血管外科专家们针对VTE的诊疗现状及焦点问题展开了一系列高规格、近距离交流,共同探讨了未来VTE诊治及研究方向。
 第二届积水潭血管论坛参会点评及主题讨论专家列表
其中,刘建龙主任对中国血管外科发展的总结性发言,美国匹兹堡大学医疗中心的Rabih Chaer教授关于急性髂股静脉血栓治疗的介绍,纽约大学医学中心Paul Gagne教授关于慢性静脉疾病治疗的讲解等,都让在场的血管外科医生受益良多。祝福我国的血管外科事业发展越来越好,未来希望我国的VTE诊疗水平能走在世界前沿!
第二届积水潭血管论坛参会点评及主题讨论专家列表
其中,刘建龙主任对中国血管外科发展的总结性发言,美国匹兹堡大学医疗中心的Rabih Chaer教授关于急性髂股静脉血栓治疗的介绍,纽约大学医学中心Paul Gagne教授关于慢性静脉疾病治疗的讲解等,都让在场的血管外科医生受益良多。祝福我国的血管外科事业发展越来越好,未来希望我国的VTE诊疗水平能走在世界前沿!
 北京积水潭医院血管外科科主任
主要研究方向:血管外科专业
现任北京医学会血管外科分会、血栓与止血分会、创面修复分会常委,北京医师协会血管与腔内血管外科专家委员会常委,北京中西医结合血管外科学会常委,中华医学会组织工程与血管外科专业委员会常委,中国医师协会血管外科专业委员会常委,中华损伤与修复杂志、血管外科杂志、山东医药等杂志编委
北京积水潭医院血管外科科主任
主要研究方向:血管外科专业
现任北京医学会血管外科分会、血栓与止血分会、创面修复分会常委,北京医师协会血管与腔内血管外科专家委员会常委,北京中西医结合血管外科学会常委,中华医学会组织工程与血管外科专业委员会常委,中国医师协会血管外科专业委员会常委,中华损伤与修复杂志、血管外科杂志、山东医药等杂志编委


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#积水潭#
78
#梅斯#
60
学习了一下新知识
195
高水平论坛
136
积血潭
124