盘点:心血管疾病介入治疗指南与共识(下)
2016-08-26 MedSci MedSci原创
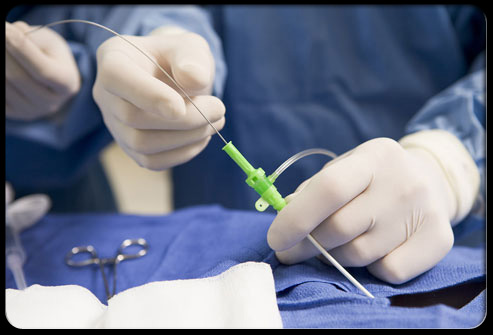
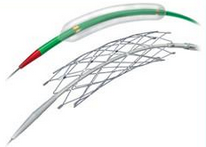
十、2013 介入放射科抗菌药物使用指南(草案)介入放射学技术在我国开展巳有30年历史,巳成为目前诊断和治疗多种疾病的重要手段。由于介入手术创口、创伤较小,越来越受到医师和患者的欢迎。当前介入手术与外科手术一样也存在抗菌药物预防性使用不合理现象,如使用率偏高、用药时间不合理、疗程过长等,需进一步规范管理,加强培训,加大干预力度,促进抗菌药物合理使用。(文章详见——介入放射科抗菌药物使用指

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗指南#
61
文章很好值得关注
89
值得学习
88
#血管疾病#
56
学习啦,谢谢分享
102
值得学习
88
谢谢指南,学习
82
阅读了。
59
继续学习
85
继续关注
62