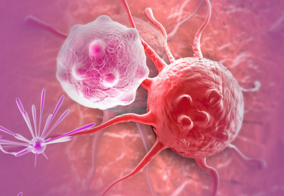
教你一分钟看懂 乳腺癌病理报告单!
2016-05-18 薛卫成 好大夫在线
拿到这样一份乳腺癌病理报告,患者心里会有很多疑问。(+) (-)符号让患者一头雾水,这些指标表示什么?重点应该看哪些指标?哪些指标会影响治疗?小医生今天邀请到北京肿瘤医院的薛教授,教您一分钟看懂乳腺癌病理报告!


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#报告单#
105
好文章,百姓也能从中学到好多医学知识
158
非常不错!
163
说的挺好,每个专业都需要它
205
讲的真好
208
讲的很清楚了
222
值得学习
129
的确好文章
111
学习一下!
133