Int J Mol Med:研究发现ZNF571-AS1或参与了急性髓系白血病的发生
2017-09-01 MedSci MedSci原创
急性髓系白血病(AML)是一种高度异质性的恶性血液病,其预后差异较大。既往研究表明,长非编码RNAs(lncRNAs)在AML的发生发展中发挥了重要作用,因此或可作为预测AML的潜在标志物。然而,利用lncRNA作为AML预后标志物及其具体作用机制目前尚未明了。在本研究中,在构建了lncRNA-lncRNA共表达网络(LLCN)后,研究人员使用AML的RNA-seq V2数据计算lncRNAs和m
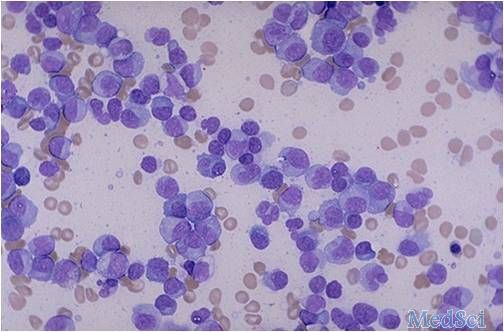
急性髓系白血病(AML)是一种高度异质性的恶性血液病,其预后差异较大。既往研究表明,长非编码RNAs(lncRNAs)在AML的发生发展中发挥了重要作用,因此或可作为预测AML的潜在标志物。然而,利用lncRNA作为AML预后标志物及其具体作用机制目前尚未明了。
在本研究中,在构建了lncRNA-lncRNA共表达网络(LLCN)后,研究人员使用AML的RNA-seq V2数据计算lncRNAs和mRNA的表达水平。共确定了8个与 AML预后相关的lncRNA,与患者的生存率显著相关(P≤0.05)。随后,构建预后相关的lncRNA分子通路来解释AML预后模块的功能机制。结果表明,这些预后分子参与了AML通路、趋化因子信号通路和Wnt信号通路。此外,在这些预后模块中探究lncRNA发现ZNF571-AS1或通过调节KIT及STAT5经JAK/ STAT通路参与AML的发生发展。
总之,本研究不仅提供了潜在的lncRNA模块作为AML的预后标志物,也为进一步探究lncRNAs的分子机制提供了新的见解。
原始出处:
Jia-Qi Pan, Yan-Qing Zhang, et al., lncRNA co-expression network model for the prognostic analysis of acute myeloid leukemia. Int J Mol Med. 2017 Mar; 39(3): 663–671. Published online 2017 Feb 13. doi: 10.3892/ijmm.2017.2888.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#研究发现#
58
#髓系白血病#
66
#Med#
55