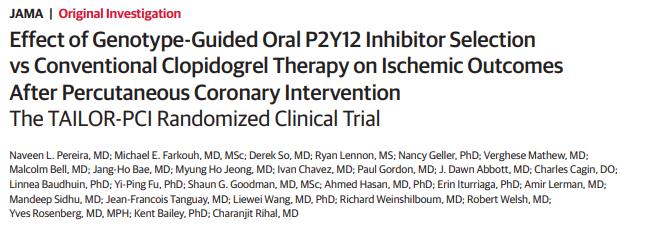
JAMA:CYP2C19Lof携带患者与基因型指导的抗血小板药物治疗策略
2020-08-26 MedSci原创 MedSci原创
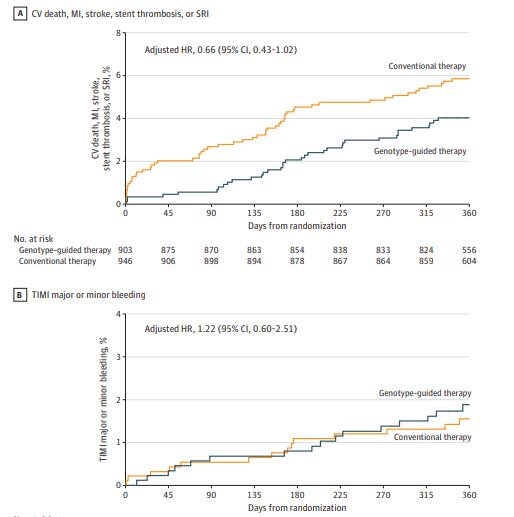
研究认为,对于携带CYP2C19 LOF突变的急性冠状动脉综合征或稳定型冠状动脉疾病患者,根据基因型指导选择P2Y12抑制剂治疗策略效果不显著
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抗血小板药#
63
#基因型#
81
#CYP2C19#
72
#血小板药物#
73
好资料
140
学习了
142
相关资讯请继续分享,谢谢
134
很好很详细,谢谢分享
144
学习了
148
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
40