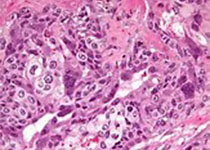
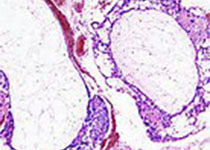
Clin cancer res:FTD/TPI+伊立替康+贝伐单抗联合治疗晚期消化道肿瘤的疗效和安全性
2020-04-06 QQY MedSci原创
FTD/TPI+伊立替康+贝伐单抗联合治疗转移性结直肠癌(mCRC)的安全性、药物动力学和FTD抗肿瘤活性目前尚不明确。
方法:本试验是一个Ib期临床试验,分为两个部分:剂量递增阶段(3+3设计),晚期胃肠道肿瘤患者接受FTD/TPI(每疗程的前5天,20-35mg/m2,2次/日,14天/疗程)和伊立替康(第1天,120–180mg/m2)。剂量扩增阶段,mCRC患者接受最大耐受剂量的FTD/TPI和伊立替康联合贝伐单抗(第1天,5mg/kg)。
结果:共招募了50位患者:26位分至6个剂量递增队列,24位分至剂量扩增阶段。在剂量递增阶段观察到2例剂量限制性毒性作用(疲劳和中性粒细胞减少),FTD/TPI的MTD为25mg/m2(2次/日)联合伊立替康 180mg/m2。在剂量扩增阶段,83%(20/24)的患者发生过任何原因的3级及以上的不良反应(AEs),最常见的是中性粒细胞减少(42%)、白细胞减少(25%)和腹泻(12%),分别导致29%、17%、4%的患者的给药中断、修改和终止。无治疗相关死亡。3位(12%)患者获得部分缓解,16位(67%)患者病程稳定持续超过4个月。中位无进展存活期为7.9个月。
结论:在本I期试验中,耐受性和疗效结果支持进一步在既往治疗过的mCRC患者中评估FTD/TPI+伊立替康+贝伐单抗联合方案的应用价值。
原始出处:
Anna M. Varghese, et al. Phase I Study of Trifluridine/Tipiracil Plus Irinotecan and Bevacizumab in Advanced Gastrointestinal Tumors. Clinical Cancer Research. April 2020. DOI: 10.1158/1078-0432.CCR-19-2743
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疗效和安全性#
72
#FTD/TPI#
66
#联合治疗#
56
#消化道#
65
#贝伐#
58
#FTD#
65
谢谢梅斯提供这么好的信息,学到很多
96