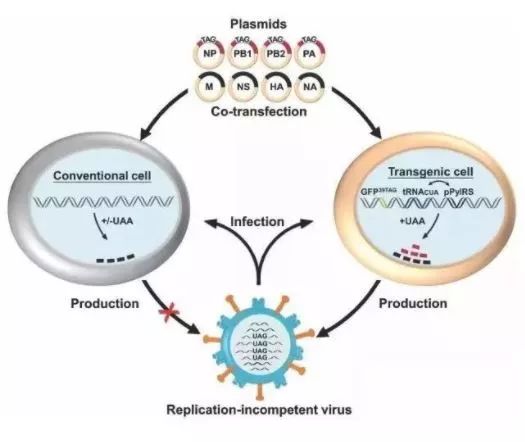
基因密码神来之笔,重磅流感活疫苗诞生记——专访北大药学院长周德敏教授
2018-01-10 佚名 学术经纬
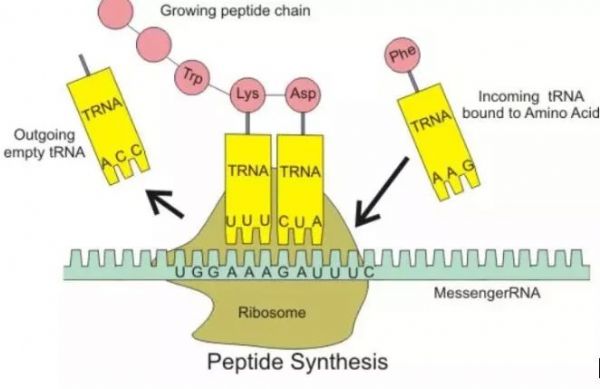
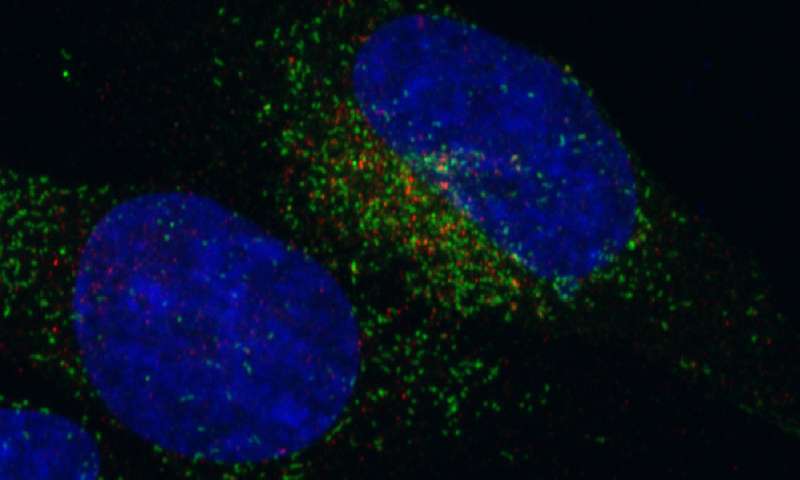
然而,免疫探索之路依然任重道远。流感病毒是最容易影响普通人健康的病原体之一,而小小的流感病毒所导致的恐慌和威胁,也从未停下过侵扰人类的脚步。至今,治疗流感尤其是重症患者的药物疗效依然有限,流感疫苗仍是普通人群最应关注的预防手段。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#活疫苗#
80
#专访#
103
#药学院#
78
好
81
#重磅#
67
谢谢分享.学习了
119
好好好好好好好好
90