Heart:SVT患者接受辅助医务人员治疗很安全!
2017-09-26 王淳 环球医学
2017年9月,发表在《Heart》的一项由英国科学家进行的随机对照试验,考察了定期阵发性室上性心动过速患者接受辅助医务人员治疗的安全性和有效性。

2017年9月,发表在《Heart》的一项由英国科学家进行的随机对照试验,考察了定期阵发性室上性心动过速患者接受辅助医务人员治疗的安全性和有效性。
介绍:阵发性室上性心动过速(SVT)是紧急入院的常见原因。腺苷是一种有效的治疗方法。至今,没有研究直接比较腺苷治疗的急性SVT患者的辅助医务人员治疗vs医院提供治疗。
方法:比较辅助医务人员SVT治疗和出院vs基于传统急诊的治疗的随机对照试验。将具有结构性心脏病或对腺苷禁忌的患者排除。研究人员比较了出院时间、随访管理、成本和患者满意度。
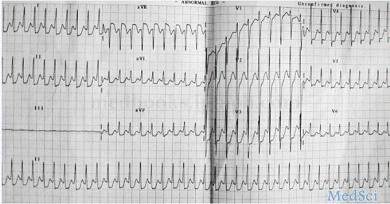
结果:纳入86例患者:44例随机分配到辅助医务人员驱动的腺苷(PARA)组,42例分配到常规治疗(ED)组。PARA组给予腺苷的37例患者中,81%成功终止了心动过速。辅助医务人员的ECG诊断与两名电生理医生的ECG诊断具有98%的相关性。两组没有患者发生不良事件。PARA组比ED组的出院时间短(125分(范围55~9513)vs 222分(72~26153),P=0.01),该治疗策略具有更大成本效果(£282 vs £423,P=0.01)。多数患者更倾向于该管理方法。辅助医务人员治疗和出院并不影响患者接受心律失常和心脏病随访持续管理的可能性。
结论:SVT患者能有效和安全地接受经过培训的辅助医务人员传递的腺苷治疗。实施辅助医务人员传递的急性SVT治疗具有降低医疗成本而不影响患者治疗的潜力。
原始出处:
Honarbakhsh S, Baker V, Kirkby C, et al. Safety and efficacy of paramedic treatment of regular supraventricular tachycardia: a randomised controlled trial. Heart. 2017 Sep;103(18):1413-1418. doi: 10.1136/heartjnl-2016-309968. Epub 2016 Sep 9.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#SVT#
99
#医务人员#
103
#ART#
69
#HEART#
68
射频消融治疗
96