Blood:CD19 CAR-T细胞疗法明显提高ALL患者的无事件存活期
2019-02-09 MedSci MedSci原创
中心点:基础血小板计数、LDH和淋巴细胞耗竭方案均会影响CD19 CAR-T细胞治疗后获得MRD阴性的完全缓解的患者的无事件存活期。CD19 CAR-T细胞治疗后进行同种异体HCT,患者耐受性好,还有望延长患者的无事件存活期。摘要:特异性表达CD19嵌合抗原受体(CAR)的自体T细胞可提高复发性/难治性急性B淋巴细胞白血病(B-ALL)患者的微小残留病阴性的完全缓解(MRD-CR)率。但是,与CA
基础血小板计数、LDH和淋巴细胞耗竭方案均会影响CD19 CAR-T细胞治疗后获得MRD阴性的完全缓解的患者的无事件存活期。
CD19 CAR-T细胞治疗后进行同种异体HCT,患者耐受性好,还有望延长患者的无事件存活期。
摘要:
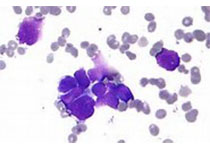
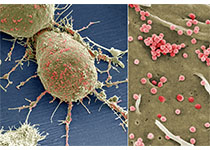
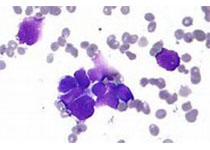
特异性表达CD19嵌合抗原受体(CAR)的自体T细胞可提高复发性/难治性急性B淋巴细胞白血病(B-ALL)患者的微小残留病阴性的完全缓解(MRD-CR)率。但是,与CAR-T细胞治疗后持续缓解相关的细胞因子尚未完全明确。
Kevin A. Hay等人对参与评估淋巴细胞耗竭化疗后予以CD19 CAR-T细胞治疗的I/II期临床试验(NCT01865617)所有复发性/难治性B-ALL患者进行分析研究。53位接受CD19 CAR-T细胞治疗的患者中有45位(85%)获得MRD-阴性的完全缓解。
Kevin A. Hay,et al.Factors associated with durable EFS in adult B-cell ALL patients achieving MRD-negative CR after CD19 CAR-T cells. Blood 2019 :blood-2018-11-883710; doi: https://doi.org/10.1182/blood-2018-11-883710
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CAR-#
86
#Car-T细胞疗法#
0
#ALL#
73
#CD19#
68
#T细胞疗法#
82
#存活期#
93